Application of ECMO in Upper Airway Obstruction and Case Analysis
- 1. Department of Otolaryngologeal Head and Neck Surgery, the 6th Medical Center of Chinese PLA General Hospital, China
- 2. National Clinical Research Center for Otolaryngologic Diseases, China
Abstract
Extracorporeal membrane oxygenation (ECMO) is a life-supporting cardiopulmonary adjuvant therapy primarily used for respiratory and circulatory disorders. Upper airway obstruction is a critical emergency in otolaryngology. The application of ECMO in acute upper airway obstruction provides a novel approach for managing such conditions, improving rescue success rates, and is worthy of reference and promotion among ENT physicians.
Keywords
• Airway Obstruction; Dyspnea; ENT Physicians; Otolaryngology; ECMO
Citation
Chen L, Zong L, Li S, Yuan L, Gao G, et al. (2026) Application of ECMO in Upper Airway Obstruction and Case Analysis. Ann Otolaryngol Rhinol 13(2): 1384.
INTRODUCTION
ECMO (extracorporeal membrane oxygenation) is a cardiopulmonary support technology that provides life sustaining oxygenation and circulation for patients with severe respiratory or cardiac failure. Initially developed from cardiopulmonary bypass (CPB) techniques, ECMO has been widely applied in conditions such as acute respiratory distress syndrome (ARDS), severe pneumonia, pulmonary contusion, status asthmaticus, lung transplantation, acute heart failure, pulmonary embolism, cardiogenic shock, and as a bridge to cardiac transplantation or ventricular assist devices. With advancements in ECMO technology and materials, its clinical applications continue to expand. In otolaryngology, ECMO has emerged as a critical intervention for acute upper airway obstruction. This article reports two successful cases of ECMO-assisted management of upper airway obstruction and discusses its clinical implications.
CLINICAL DATA
Case 1
A 54-year-old female presented with a neck mass persisting for 10 months and progressive dyspnea for 20 days. Initial diagnosis at a local hospital indicated a thyroid mass, but medical therapy was ineffective. The mass enlarged, compressing the trachea and causing worsening dyspnea.
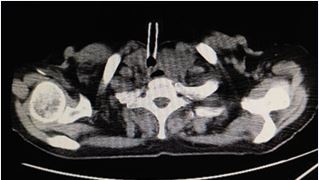
Examination: Physical examination revealed a protruding anterior neck mass with ill-defined borders, mobile upon swallowing. Subcutaneous edema was noted in the left submandibular region Neck ultrasound revealed diffuse thyroid enlargement compressing the trachea, esophagus, and left common carotid artery. CT confirmed a large left thyroid lobe mass, suspected malignancy, with tracheal compression and left jugular vein involvement (Figure 1). Thyroid function tests showed elevated thyroxine (175.6 nmol/L), suppressed TSH (0.12 mU/L), and elevated anti-thyroglobulin (62.3 IU/mL) and anti-TPO antibodies (217.7 IU/mL).
Figure 1 The lesion invades and compresses the trachea, resulting in luminal stenosis, and extends through the membranous portion into the tracheal lumen, partially obstructing the airway (yellow arrow). The left common carotid artery is completely encased by the tumor (red arrow), while the left internal jugular vein is infiltrated with luminal compression and stenosis (blue arrow).
Diagnosis: Large thyroid mass with grade II dyspnea.
Intervention: Under general anesthesia, a V-V ECMO assisted thyroid biopsy and tracheostomy were performed. Intraoperative resection of anterior thyroid tissue for pathological diagnosis, with subsequent tracheal exposure and tracheostomy. Pathological examination confirmed diffuse large B-cell lymphoma (germinal center origin, Ann Arbor stage IV XB). Postoperatively, the patient was transferred to hematology for further treatment. Follow-up CT at two months showed significant tumor regression and a stable tracheostomy (Figure 2). Electronic laryngoscopy showed no obvious tracheal stenosis (Figure 3).Follow-up is ongoing
Figure 2 Neck CT demonstrates significant post-treatment reduction in the left thyroid lobe mass, which no longer causes significant compression or obstruction of the cervical trachea. A tracheostomy has been performed.
Figure 3 Laryngoscopy reveals left vocal cord paralysis with normal right vocal cord mobility and no significant tracheal stenosis.
Case 2
A 15-year-old female with a history of tracheal tumor resection five months prior presented with worsening dyspnea over 20 days. Initial surgery involved tracheal sleeve resection and end-to-end anastomosis for a granular cell tumor.
Examination: Physical examination revealed inspiratory dyspnea with mild sternal retractions. Laryngoscopy revealed a 4 mm scar-induced tracheal stricture. Normal vocal cord mobility (Figure 4). Neck CT confirmed a 1.5 cm tracheal stenosis with a 4 mm narrowest diameter (Figure 5).
Figure 4 Laryngoscopy demonstrates symmetric vocal cord mobility without glottic stenosis. A circumferential scar-induced stenosis (approximately 4mm in diameter) is observed in the subglottic cervical trachea.
Figure 5 Preoperative 3D airway CT reconstruction identifies critical stenosis at the cervical trachea (arrow).
Intervention: Under local anesthesia, a tracheostomy was performed with an incision made above the tracheal stenosis. A 5mm endotracheal tube was inserted to induce general anesthesia. Sequential dilation of the stenotic segment was then performed using 5.5mm and 6.0mm endotracheal tubes with balloon inflation. During the attempt to replace the tube with a tracheostomy cannula, successful placement was not achievable, prompting emergent veno-venous ECMO (V-V ECMO) support. After establishing stable ECMO circulation, a 7.0mm tracheostomy tube was successfully placed under bronchoscopic guidance. The patient maintained stable vital signs postoperatively. At the 3-month follow-up, the tube was exchanged for a No. 6 metal tracheostomy cannula. Currently, the patient remains with the metal tracheostomy tube under ongoing follow-up observation.
DECLARATIONS
This study was approved by the ethics committee of the 6th Medical Center of Chinese PLA General Hospital. All methods were carried out in accordance with relevant guidelines and regulations. Patients were consented by an informed consent process that was reviewed by the Ethics Committee of 6th Medical Center of Chinese PLA and certify that the study was performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki. all data used during the study are available from the corresponding author by request.
DISCUSSION
Extracorporeal Membrane Oxygenation (ECMO), derived from cardiopulmonary bypass (CPB) used in cardiac surgery, is a bionic method of artificial blood oxygen exchange. It involves diverting venous blood to an external membrane oxygenator before reinfusing it into the body, providing cardiopulmonary support for patients with respiratory or circulatory failure [1]. The ECMO circuit consists of arterial/venous cannulas, tubing, a reservoir, a pump (artificial heart), a membrane oxygenator (artificial lung), a heat exchanger, connectors, a bridge between drainage and return lines, and a monitoring system [2].
ECMO has two primary modes: veno-venous ECMO (VV-ECMO) and veno-arterial ECMO (VA-ECMO). VV ECMO pumps oxygenated blood into the venous system, providing only respiratory support, and is primarily used for respiratory failure. VA-ECMO delivers oxygenated blood directly into the arterial system, offering both oxygenation and circulatory support by partially or fully replacing cardiac function, reducing myocardial workload. Thus, VA-ECMO is applicable in both respiratory and circulatory failure.
Initially, ECMO was mainly used for cardiopulmonary failure. However, with advancements in technology, biomaterials, and clinical exploration, its indications have expanded. Current applications broadly fall into four categories: circulatory failure, respiratory failure, ECMO assisted CPR, and other conditions requiring circulatory support [3].
Upper airway obstruction is a critical emergency with high mortality, demanding prompt diagnosis and intervention. Thyroid-related airway obstruction presents unique challenges. Unlike laryngotracheal stenosis— where tracheostomy is often definitive—thyroid diseases (e.g., goiter or malignancy) may obscure the trachea, increasing procedural risks. Alternatives include:
1. Conservative management oxygen, steroids, antibiotics): Suitable for mild obstruction caused by reversible edema (e.g., thyroiditis or lymphoma).
2. Endotracheal intubation or intubation followed by tracheostomy. This approach is suitable for most cases of airway obstruction caused by thyroid diseases [4]. After nasotracheal or orotracheal intubation, subsequent diagnostic or therapeutic measures are implemented. If the underlying condition can be controlled within a short period (1-2 weeks), resulting in thyroid size reduction and relief of airway compression, tracheostomy may be avoided. However, if airway compression persists, tracheostomy becomes necessary. Performing tracheostomy after intubation offers greater safety and allows for biopsy of pathological tissues during tracheal exposure, facilitating definitive diagnosis and guiding further treatment. Nevertheless, endotracheal intubation carries inherent risks of airway irritation. For patients with severe airway stenosis (tracheal diameter <4mm), intubation attempts may provoke airway spasm or edema, potentially leading to failed intubation and life-threatening asphyxia.
3. Tracheal stenting: Airway stent placement can alleviate malignant thyroid-related airway obstruction, serving as a bridge to definitive therapies like chemoradiation [5]. However, this approach carries significant limitations including risks of glottic stenosis, stent migration, tracheoesophageal fistula formation, and difficult stent removal, which restrict its clinical utility [5]. Beyond the aforementioned approaches, ECMO currently offers an innovative solution for managing upper airway obstruction. By providing extracorporeal oxygenation support, ECMO effectively circumvents the risks associated with endotracheal intubation, tracheostomy, and airway stent placement, thereby significantly improving resuscitation success rates. ECMO circumvents the hazards of intubation/tracheostomy in high-risk cases. The first case in our study involved a patient with severe airway stenosis caused by compression from a massive thyroid tumor. Under conventional emergency protocols, the only option would have been high-risk endotracheal intubation - a procedure with significant potential for failure and fatal asphyxia in such cases of tumor-invaded, critically narrowed airways. By employing ECMO technology, we effectively resolved this clinical challenge, significantly enhancing procedural safety and ensuring patient survival. The second case in our series involved a patient with tracheal stenosis who developed acute airway crisis during general anesthesia. During the planned procedure of dilatation and tracheostomy tube exchange, unexpected complete lumen occlusion occurred due to stent failure, making recannulation impossible. In conventional practice, failure to immediately reestablish airway access under such circumstances would inevitably lead to fatal asphyxia in this apneic, anesthetized patient. The timely initiation of ECMO in this critical scenario proved lifesaving - by maintaining oxygenation, it created a vital window for the surgical team to methodically identify the tracheal lumen and successfully place a new tracheostomy tube, thereby ensuring complete procedural safety. The successful management of these two cases through ECMO application has pioneered a novel therapeutic strategy for acute upper airway obstruction, significantly expanding the clinical scope of ECMO utilization. However, as a relatively emerging technology, ECMO remains limited to tertiary medical centers and its widespread adoption is constrained by substantial costs. Furthermore, ECMO carries significant complication risks including hemorrhage, thromboembolism, infection, acute kidney injury, and neurological impairment - with some adverse events occurring in 30-70% of cases [6]. While ECMO represents a groundbreaking advancement in airway emergency management, its implementation requires: (1) rigorous patient selection, (2) comprehensive risk-benefit analysis, and (3) meticulous procedural preparation to ensure both safety and therapeutic efficacy.
CONCLUSION
Acute upper airway obstruction requires immediate, effective intervention. ECMO offers a transformative rescue strategy but warrants judicious application. Further studies are needed to refine its role in otolaryngologic emergencies.
REFERENCES
- Brogan TV, Thiagarajan RR, Rycus PT, Bartlett RH, Bratton SL. Extracorporeal membrane oxygenation in adults with severe respiratory failure: a multi-center database. Intensive Care Med. 2009; 35: 2105-2114.
- Bartlett RH. ECMO: The next decade. ASAIO J. 2022; 68: 291-299.
- Combes A. ECMO for severe ARDS. JAMA. 2018; 320: 2251-2264.
- Schmidt M. Venoarterial ECMO in cardiogenic shock. Eur Heart J. 2019; 40: 2672-2684.
- Ramanathan K. ECMO in perioperative emergencies. J Cardiothorac Vasc Anesth. 2020; 34: 257-265.
- Fletcher K. Complications of neonatal ECMO. Semin Perinatol. 2018; 42: 68-79.