Application of Individual Cosmetic Incisions in Superficial Parotidectomy for Benign Tumors
- 1. Department of Stomatology, Jiangsu Province Hospital, The First Affiliated Hospital of Nanjing Medical University, China
Abstract
Objective: This study aimed to evaluate the application of cosmetic incisions for benign tumors located in the superficial lobe of the parotid gland and to identify the optimal incision type based on tumor location.
Methods: A retrospective analysis was conducted involving 114 patients with benign parotid tumors who underwent parotidectomy utilizing “V-shaped,” pre-auricular crutch, or “N-shaped” incisions. Post-operative outcomes were meticulously recorded, including operation time, drainage volume, incidence of temporary facial paralysis, occurrence of salivary fistulae, and patient satisfaction levels
Results: All surgical procedures were successful, with no significant recurrence of tumors observed during the follow-up period ranging from 6 to 18 months. The rates of temporary facial paralysis and salivary fistula did not demonstrate any significant differences among the various incision types. Notably, patient satisfaction scores were significantly higher for pre-auricular crutch incisions (10.0) compared to “V-shaped” (9.0) and “N-shaped” (8.0) incisions. Subgroup analyses indicated that “V-shaped” incisions proved superior for small tumors situated in the middle parotid area concerning both operation time and drainage volume
Conclusion: The selection of an appropriate cosmetic incision tailored to tumor characteristics can enhance postoperative satisfaction levels. While “N-shaped” incisions fulfill clinical requirements effectively, “V-shaped” or pre-auricular crutch incisions may be favored for improved patient satisfaction— particularly for small to medium-sized tumors located in specific areas
Keywords
• Cosmetic; Incisions; Parotidectomy; Patient Satisfaction
CITATION
Zhu L, Zhuang H, Zhang J, Bu S, Wang C (2025) Application of Individual Cosmetic Incisions in Superficial Parotidectomy for Benign Tumors. Ann Otolaryngol Rhinol 12(1): 1353.
INTRODUCTION
Parotid gland tumors are one of the most common diseases in dentistry, with 80% of them being benign tumors, and 90% located in the superficial lobe of the parotid gland [1]. Surgical resection is the preferred treatment for these tumors, and the traditional surgical approach is an “S-shaped” incision. This incision provides good exposure of the salivary gland area and facial nerve protection, and is widely used in clinical practice [2,3]. Nevertheless, patients often complain about neck scars after the surgery, especially young female patients who care about their appearance [4]. To address this issue, Appiani et al., first applied a facial wrinkle incision (N-shaped incision) [5], to the removal of salivary gland tumors. This incision includes preauricular, post-auricular, and hairline incisions, which improves the cosmetic outcome by hiding scars behind the ear and in the hairline.
Several studies [4,6], both domestically and internationally has represent that the “N-shaped” incision can achieve the same therapeutic effect as the “S-shaped” incision while achieving better cosmetic outcomes. However, other scholars have found that longer incisions increase the probability of skin necrosis after flap surgery, and hairline incisions may lead to alopecia or hypertrophic scars [7], especially for male patients with short hair. In order to improve the cosmetic effect, A minor incision, such as the “V”-shaped incision [8,9], preauricular crutch incision [10], postauricular hairline incision [11,12], postauricular incision [13], and Endoscopic parotid surgery [14], has been designed. However, there are fewer reports on how to pick up the appropriate cosmetic incision. Many surgeons face challenges in determining the appropriate cosmetic incision for a specific situation, often abandoning it after an initial attempt, even experienced surgeons encounter such difficulties.
Hence, the study centered on retrospectively analyzing patients with benign salivary gland tumors treated at the First Affiliated Hospital of Nanjing Medical University between 2017 and 2019. The aim was to explore various cosmetic incision options for salivary gland tumors of varying sites and sizes, along with their clinical implications.
MATERIALS AND METHODS
General information
The study is subscribed by the Jiangsu Province Hospital Ethics Committee, Ethics Number 2023-SR-215. A total of 127 patients with parotid gland tumors who underwent cosmetic incisions at the Department of Stomatology, the First Affiliated Hospital of Nanjing Medical University between January 2015 and June 2019 were analyzed retrospectively. Inclusion criteria: a) negative history of previous injury in the surgical area, b) initial surgery for salivary gland tumor, c) surgery performed via cosmetic incision, d) Pathological diagnosis of benign tumors, e) patients with intact cognitive function who were able to complete the assessment independently. Exclusion criteria: a) Recurrent salivary gland tumors, b) surgery performed via conventional “S” incision, c) Pathological diagnosis of a malignant tumors, d) Patient with cognitive impairment or unable to complete the assessment independently. All patients must sign informed consent forms prior to surgery. 13 of the 127 patients had malignant salivary gland tumors, including 4 cases of adenoid cystic carcinoma, 3 cases of mucoepidermoid carcinoma, 2 cases of acinar cell carcinoma, 1 case of squamous cell carcinoma, 2 cases of myoepithelial carcinoma, and 1 case of malignant pleomorphic adenoma. A total of 114 patients with benign salivary gland tumors were included after excluding these cases.
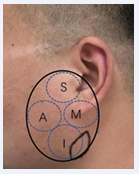
According to the location of the tumor in the salivary gland, it was divided into four regions as shown in Figure 1:
Figure 1: Tumor location division within the parotid gland: superior, inferior, anterior, and middle zone
Superior (S-zone): the lowest point in the salivary gland area is above the earlobe; Inferior (I-zone): the highest point in the salivary gland area is below the earlobe; Anterior (A-zone): the posterior-most point in the salivary gland area is located behind the mandibular bone; other areas are referred to as the middle (M-zone) region, and the cross-region is mainly determined by the area occupied by the tumor.
Tumors were classified as small (4cm) based on their diameter. Preoperatively, the incision approach was determined according to the location, size, and activity of the salivary gland tumors, and the patient’s consent was obtained through communication with the patient.
Surgical Incisions
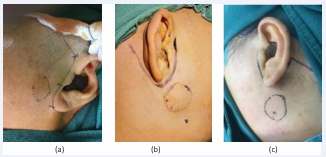
There are three different types of cosmetic incisions that are used for the procedure as shown in Figures 2.
Figure 2: (a) “Preauricular crutch” Incision; (b) “V-shaped” incision; (c) “N-shaped” incision
For example, for small-diameter tumors in the M region, the available options were “V-shaped” incision, “N-shaped” incision, and traditional “S” incision. Ultimately, the “N-shaped” incision was selected in 64 patients, the “V-shaped” incision was selected in 34 patients, and the “preauricular crutch” incision was selected in 16 patients. For details on patient demographics, please refer to Table 1.
Table 1: Patients basic information
|
|
"N-shaped" incision |
"V-shaped" incision |
"preauricular crutch" incision |
P |
|
Gender |
|
|
|
0.126 |
|
Male |
37 |
13 |
10 |
|
|
Female |
27 |
21 |
6 |
|
|
Age(year) |
55.0 [39.8, 65.0] |
42.0 [34.2, 49.5] |
30.0 [24.8, 32.5] |
<0.001 |
|
Diameter |
2.5 [1.8, 3.4] |
1.8 [1.2, 2.2] |
2.0 [1.7, 2.3] |
<0.001 |
|
Location |
|
|
|
|
|
S-zone |
1 |
0 |
16 |
|
|
A-zone |
10 |
5 |
0 |
|
|
I-zone |
32 |
0 |
0 |
|
|
M-zone |
21 |
29 |
0 |
|
|
Operation method |
|
|
|
|
|
ECD |
20 |
25 |
10 |
|
|
PSP |
30 |
9 |
6 |
|
|
SP |
10 |
0 |
0 |
|
|
TP |
4 |
0 |
0 |
|
|
Pathology |
|
|
|
|
|
pleomorphic adenoma |
20 |
20 |
7 |
|
|
Adenolymphoma |
26 |
6 |
3 |
|
|
Basal cell adenoma |
7 |
3 |
2 |
|
|
Hemangioma |
1 |
1 |
1 |
|
|
Lymphoepithelial cyst |
2 |
1 |
2 |
|
|
Branchial cyst |
2 |
2 |
1 |
|
|
Schwannoma |
1 |
0 |
0 |
|
|
Lipomyoma |
1 |
0 |
0 |
|
|
Epidermal cyst |
2 |
0 |
0 |
|
|
Calcified epithelioma |
0 |
1 |
0 |
|
|
salivary duct cyst |
1 |
0 |
0 |
|
|
Parotid cyst |
1 |
0 |
0 |
|
(a). “Preauricular crutch” Incision: For parotid gland masses located in the S area with a diameter less than 2cm and good mobility, a linear incision was made in front of the earlobe that extended obliquely towards the hairline.
(b). “V” Incision: For parotid gland masses located in the shallow lobe M area with a diameter less than 2cm and good mobility, a straight incision was made along the ear groove from the upper part of the ear to the earlobe.
(c) “N” Incision: This incision was more widely used for masses located in different positions and sizes. The approach began with the pre-auricular incision. The incision descends towards the posterior auricular groove, and following a circular arc shape towards the back. Finally, the incision parallel to the hairline at the midpoint of the external auditory canal.
Postoperative treatment
After surgery, cefuroxime sodium 1.5g is administered intravenously twice daily for two days to prevent infection. In order to avoid salivary fistula, pressure dressing was continued for one week after removing the negative pressure drainage vessel, and patients were advised to avoid sour and spicy food for one month.
Postoperative observation
Duration of surgery, drainage volume, and the occurrence of postoperative complications, including temporary facial palsy and salivary fistula are observed during the follow-up period of 6-18 months for both groups of patients. At 6 months postoperatively, patients’ satisfaction with the incision scar was analyzed based on subjective evaluations. Patients are monitored for dry mouth and tumor recurrence at 6-18 months postoperatively. Specifically, the following criteria are used for assessment:
1) Temporary facial palsy: Patients were evaluated using the HB grading scale [15], one week after surgery. If temporary facial palsy was present, nutritional and neurological treatments and rehabilitation training were given. Further evaluation was performed 6 months after surgery.
2) Salivary fistula: The number of cases of salivary fistula was evaluated, with no occurrence of salivary fistula being recorded as 0, and the occurrence of salivary fistula being recorded as 1.
3) Subjective satisfaction with incision scar after surgery: Patients used the VAS rating scale to score their satisfaction levels, with 0 representing extremely dissatisfaction and 10 representing extremely satisfaction. This evaluation was conducted 3 months after surgery.
4) Patients underwent salivary gland ultrasound to determine if there were any signs of tumors recurrence at 6-18 months postoperatively.
Statistical analysis
Data were entered into SPSS 24.0 software for analysis. If the quantitative information conformed to normal distribution, it was represented as x±s, and t-test was used for comparison between groups. If the quantitative data did not follow a normal distribution, the median (interquartile range) is used, and group comparisons are made using a rank sum test. Count data were represented as a percentage, and the chi-square test was used for comparisons between groups. A P-value less than 0.05 indicate a statistically significant difference.
RESULTS
There were no patients reporting or complaining of dry mouth and no signs of tumor recurrence during the follow-up period. Parotid tumors of different sites and sizes were operated with different surgical approaches and various degrees of surgical difficulty. Therefore, we compared parotid gland tumors using the same surgical technique but different incisions in the statistical analysis. The specific data is as follows:
Surgical-related Indicators
The basic surgical information of the three patient groups is presented in Table 2. In this study, the “N-shaped” incision group exhibited significantly longer surgery times and higher postoperative drainage volumes compared to both the “pre-auricular crutch” incision group and the “V-shaped” incision group. This can be attributed to factors such as larger tumor diameters, requirements for extensive flap areas, and dissection of the facial nerve during surgery, as shown in Table 1. Moreover, the “V-shaped” incision group also demonstrated prolonged surgery times and increased postoperative drainage volumes when contrasted with the “pre-auricular crutch” incision group. This indicates that the “V-shaped” incision was associated with greater complexity and trauma relative to the “pre auricular crutch” approach.
Table 2: Statistical comparison of operation time and postoperative drainage among three groups of patients
|
groups |
N |
drainage volume /mL |
surgery time /min |
|
"Preauricular crutch" Incision |
16 |
20.0 [15.0, 26.2] |
47.5 [38.8, 65.0] |
|
"V-shaped” incision |
34 |
30.0 [21.2, 35.0]* |
65.0 [51.2, 70.0] * |
|
"N-shaped” incision |
64 |
40.0 [30.0, 45.0]*# |
70.0 [58.8, 82.5] *# |
|
P |
|
<0.001 |
0.004 |
The VAS scores for the three groups were expressed using a median (IQR).
* Indicates a statistically significant difference compared to group 1, P<0.05
# Indicates a statistically significant difference compared to group 2, P<0.05.
As detailed in Table 1, subgroup analyses were conducted based on tumor location and size. For tumors located above the parotid gland, both the “N-shaped” and “pre-auricular crutch” incisions were considered viable options. However, only one case utilized an “N-shaped” incision while 16 cases opted for a “pre-auricular crutch” incision; thus, these categories could not be directly compared.
For tumors situated in I-zone regions, exclusively an “N-shaped” incision was employed; hence comparisons within prior groups remain non-comparable. When addressing tumors present in A and M zones, both “V-shaped” and “N-shaped” incisions were feasible choices. Further categorization based on tumor location and diameter resulted in distinct groups: small tumors located in M-zone, medium-sized tumors within M-zone, as well as small tumors found in A-zone-these are illustrated further in Tables 3.
Table 3: Small and middle tumors in M-zone and A-zone
|
Groups |
N |
age (year) |
drainage volume /mL |
surgery time /min |
|||
|
Small tumors in M-zone |
|||||||
|
"V-shaped” incision |
16 |
42.9 ± 10.3 |
30.0 (20.0 to 32.5) |
45.9 ± 8.0 |
|||
|
"N-shaped” incision |
11 |
51.1 ± 15.6 |
40.0 (32.5 to 40.0) |
57.3 ± 14.2 |
|||
|
P |
0.562 |
0.112 |
0.006 |
0.032 |
|||
|
Small tumors in A-zone |
|||||||
|
"V-shaped” incision |
5 |
37.8 ± 13.6 |
29.0 ± 5.5 |
64.0 ± 5.5 |
|||
|
"N-shaped” incision |
6 |
48.5 ± 13.2 |
32.5 ± 8.8 |
61.7 ± 11.3 |
|||
|
P |
1.000 |
0.220 |
0.461 |
0.684 |
|||
|
Middle tumors in M-zone |
|||||||
|
"V-shaped” incision |
13 |
41.0 ± 9.3 |
33.8 ± 9.8 |
75.0 (70.0 to 90.0) |
|||
|
"N-shaped” incision |
9 |
48.8 ± 16.3 |
41.1 ± 12.2 |
70.0 (65.0 to 90.0) |
|||
|
P |
0.471 |
0.170 |
0.138 |
0.589 |
|||
For patients with small to medium tumors located in the M-zone, a greater proportion opted for the “V-shaped” incision compared to the “N-shaped” incision. Conversely, among patients with small tumors situated in the A-zone, there was a tendency opposite to that observed in the M-zone group regarding preference for the “V-shaped” incision; however, this difference did not reach statistical significance. In all three groups analyzed, patients who selected the “V-shaped” incision were younger than those who chose the “N-shaped” incision. Despite this age disparity not being statistically significant, it suggests that while younger individuals may prefer aesthetically pleasing incisions, some still favor a more conservative surgical approach due to concerns over surgical risks.
In terms of postoperative outcomes for patients with small tumors in the M-zone, those undergoing surgery via the “V-shaped” incision exhibited significantly lower levels of postoperative drainage compared to their counterparts using the “N-shaped” incision. No statistically significant differences were found regarding postoperative drainage in either of the other two groups studied. This finding indicates that utilizing a “V-shaped” incision may be more beneficial in minimizing trauma within this specific cohort; however, similar advantages do not appear applicable to patients from the other two groups.
Furthermore, operation times for procedures employing a “V”-shaped incision were significantly shorter when contrasted with those performed using an “N” shaped incision within certain patient subgroups. Interestingly though, among both remaining patient cohorts utilizing “V”-shaped incisions and “N”-shaped incisions respectively—while no statistical significance emerged—the patterns suggest potential inadequacy in flap exposure achieved through “V”-incision techniques which might elevate procedural difficulty albeit marginally.
Postoperative Complications
Table 4 illustrates the postoperative complications among three groups of patients during a follow-up period of 6-18 months. None of the patients suffered from permanent facial paralysis. However, temporary facial paralysis occurred in 10 patients in the N-shaped incision group, 4 patients in the V-shaped incision group, and 1 patient in the pre-auricular incision group. The patients’ facial paralysis recovered within 3-6 months. Statistical analysis showed no significant difference in the occurrence of temporary facial paralysis and salivary fistula (P>0.05).
Table 4: Statistical comparison of postoperative complications among three groups of patients
|
Groups |
N |
Facial paralysis |
Salivary fistula |
|
"Preauricular crutch" Incision |
16 |
1 |
0 |
|
"V-shaped” incision |
34 |
4 |
5 |
|
"N-shaped” incision |
64 |
10 |
9 |
|
P |
|
0.587 |
0.271 |
Postoperative Satisfaction
Patients were surveyed regarding their cosmetic satisfaction six months postoperatively. Patients in the cosmetic incision group exhibited scars that were strategically positioned within natural folds either anterior or posterior to the ear, as well as within the hairline. Even when scars were discernible, they were not situated in prominently visible areas. All patients reported being satisfied with their appearance, achieving a median satisfaction score of 9 [IQR 7-10]. No statistically significant difference was observed between the “ pre-auricular crutch” incision group and the “ V-shaped” incision group (P = 0.525). In contrast, patients in the “N-shaped” incision group demonstrated significantly lower levels of satisfaction compared to both the “pre-auricular hairline” and “V-shaped” incision groups. Notably, participants in the aforementioned groups—“pre-auricular crutch” and “V-shaped” indicated higher postoperative satisfaction levels than those categorized under the “N-shaped” incision group.
Table 5: Postoperative Satisfaction Statistics of Three Groups of Patients
|
Groups |
N |
VAS |
P |
|
"Preauricular crutch" Incision |
16 |
9.0 [9.0, 10.0] |
<0.001 |
|
"V-shaped” incision |
34 |
10.0 [9.0, 10.0] |
|
|
"N-shaped” incision |
64 |
8.0 [6.0, 9.0]*# |
|
The VAS scores for the three groups were expressed using a median (IQR).
* Indicates that there is a statistically significant difference in score satisfaction scores compared to group 1 (P<0.05).
# Indicates that there is a statistically significant difference in score satisfaction scores compared to Group 2 (P<0.05).
DISCUSSION
Parotid gland tumors are common oral diseases, and different surgical approaches and incision styles are selected for tumors with different natures, locations, and sizes. Currently, there is a clinical consensus that Function-preserving partial salivary gland resection and tumor capsule enucleation are the first choice for the treatment of benign salivary gland tumors. Although the commonly used “S-shaped” salivary gland incision can adequately expose the salivary gland and surrounding tissues and protect the facial nerve, it cannot fully meet clinical demands due to the problem of scars in the mandibular and neck areas [16,17].
In this study, we reviewed patients with benign salivary gland tumors who underwent cosmetic incisions, including “N-shaped”, “V-shaped”, and “preauricular crutch” incisions. The results of the study also led to the common conclusion: on the premise of controlling tumor recurrence, non-increasing the operation time or trauma, and non-increasing postoperative complications, the satisfaction with incision aesthetics was significantly improved, with a median postoperative satisfaction score of 9 for all patients in the study. In addition, this study summarized the criteria for the selection of surgical incisions for benign parotid tumors of different sizes and locations through retrospective analysis. The study classified the location of the parotid gland tumors into four categories: A, M, S, I-zone.
For small tumors located in the S-zone, the “preauricular crutch” incision was deemed the optimal approach. The study included 16 patients who underwent surgery using this incision, which involves both a preauricular and hairline incision in front of the ear. The flap was limited to the parotid tissue in front of the ear. The results revealed that the operation time was significantly shorter than for the “V-shaped” and “N-shaped” incisions. This may be related to the fact that the smaller the diameter of the tumor, the less intraoperative dissection of the facial nerve. the postoperative drainage volume was significantly lower than for the other two incision types, mainly due to the smaller flap area of this incision. Moreover, the hairline incision in front of the ear reduced the postoperative aesthetic satisfaction compared to the “V-shaped” incision but had better aesthetic results than the “N-shaped” incision, with significant statistical differences. It is crucial to acknowledge that if insufficient exposure or frozen pathology suggests the presence of malignancy while utilizing the preauricular incision during surgery, it may be necessary to further enlarge the incision into an “N-shaped” or “S-shaped” configuration. These results are consistent with the findings of Zhang Q [10], that the “pre-auricular crutch” incision is suitable for patients with tumors above the earlobe level who can undergo partial parotidectomy.
In this study, “V-shaped” incision was used in 34 patients, which significantly improved the aesthetic satisfaction postoperatively by reducing the incision at the occipital hairline compared with the “N-shaped” incision and the “pre-auricular crutch” incision. This difference was statistically significant and consistent with the results of Ahn D et al. [7], who found that reducing the incision at the hairline can avoid the possibility of alopecia or hypertrophic scar formation. Furthermore, the author pointed out in the article that the extent of the flap realized in the anterior, superior, and middle (A, M, S) of the parotid gland is equivalent to the “N-shaped” incision, which can achieve complete resection of the tumor capsule. However, we believed that the absence of an incision at the occipital hairline not only reduced the exposure of the submandibular region and sternocleidomastoid muscle but also affected the exposure of the preauricular region (S) to certain extent. Therefore, the author further grouped the patients who chose the “V-shaped” incision according to the size and location of the tumor. The results showed that the “V-shaped” incision was most suitable for small-diameter tumors located in the parotid gland’s M area, which provided the most adequate exposure, reduced surgical trauma, and increased postoperative aesthetic satisfaction. For medium tumors located in M zone and small tumors located in the A zone, the “V-shaped” incision can be considered as an alternative option because this surgical incision cannot provide sufficient exposure and increase surgical difficulty, result in prolonging the operation time. The main reason for the prolongation of the operation time is that the flap of the medium tumors located in t M zone of the parotid gland and small tumors located in the A zone cannot be completely exposed at one time. Repeated flap manipulation is required during dissection of the facial nerve, which may increase the operative time.
Although the aesthetic satisfaction of the “V-shaped” incision and the “pre-auricular crutch” incision is higher than that of the “N-shaped” incision, the number of patients who chose the latter two incisions was significantly lower than that of the “N-shaped” incision group in this study due to the limitation of tumors location and size, and the difference was statistically significant. The main reason for preferring the “N-shaped” incision is that we all know that protecting the facial nerve is crucial during surgery [18,19]. The “N-shaped” incision can sufficiently expose the facial nerve trunk and each branch area, so that the facial nerve trunk can be visualized directly. To the contrary, the “V-shaped” incision and the “pre-auricular crutch” incision do not provide sufficient exposure of the facial nerve trunk and branches due to the limit of the flap range. It increases the difficulty of dissection and protection of the facial nerve to a certain extent, and it is not suitable for cases with larger parotid tumors. Over-emphasizing the pursuit of aesthetic incisions can lead to tragic occurrence of facial nerve injuries. Postoperative temporary facial nerve injury occurred in all cases during the follow-up of the study, and there was no significant difference in the safety of the three surgical incisions as long as the indications were selected correctly. This indicates that there is no significant difference in the safety of completing the three surgical incisions for surgeons with extensive experience in parotid surgery and familiarity with facial nerve anatomy.
In conclusion, we believe that cosmetic incisions are a feasible technique in parotid tumor resection. The “N-shaped” incision is suitable for all patients with benign parotid tumors, and even for some with low-grade malignant tumors. The “V-shaped” incision and “ pre-auricular crutch” incision are only applicable for patients with small-volume and limited-position benign parotid tumors, particularly for those with high aesthetic standards. However, it is essential to adhere to tumor principles for patients with malignant parotid tumors, rather than pursuing aesthetic preferences.
The primary limitation of this study is that it was a retrospective investigation. To enhance the credibility of future research, further prospective cohort studies with controlled variables are necessary. In addition, endoscopic salivary gland surgery, as a trend towards minimally invasive techniques, is expected to be increasingly adopted and implemented in future clinical practice. This approach aims to achieve surgical outcomes that are not only less invasive but also more aesthetically pleasing.
DECLARATIONS
• Ethics approval and consent to participate: This study was conducted in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments. Informed consent was obtained from all individual participants included in the study.
• Availability of data and materials: The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
• Competing interests: The authors declare that they have no conflict of interest.
Funding: this research was funded by Jiangsu Province Hospital (the First Affiliated Hospital with Nanjing Medical University) Clinical Capacity Enhancement
REFERENCES
- Kadletz L, Grasl S, Grasl MC, Perisanidis C, Erovic BM. Extracapsular dissection versus superficial parotidectomy in benign parotid gland tumors: The Vienna Medical School experience. Head Neck. 2017; 39: 356-360.
- Psychogios G, Bohr C, Constantinidis J, Canis M, Vander Poorten V, Plzak J, et al. Review of surgical techniques and guide for decision making in the treatment of benign parotid tumors. Eur Arch Otorhinolaryngol. 2021; 278: 15-29
- Weigelt F, Borzikowsky C, Hoffmann M, Laudien M. Success of minimally invasive salivary gland surgery-Quality of life, prognostic factors. Laryngoscope Investig Otolaryngol. 2020 1; 5: 832-838
- Nouraei SA, Al-Yaghchi C, Ahmed J, Kirkpatrick N, Mansuri S, Singh A, et al. An anatomical comparison of Blair and facelift incisions for parotid surgery. Clin Otolaryngol. 2006; 31: 531-534.
- Appiani E, Delfino MC. Plastic incisions for facial and neck tumors. Ann Plast Surg. 1984; 13: 335-352.
- Bär B, Mantsopoulos K, Iro H. Paradigm shift in surgery for benign parotid tumors: 19 years of experience with almost 3000 cases. Laryngoscope. 2020; 130: 1941-1946.
- Grover N, D’Souza A. Facelift approach for parotidectomy: an evolving aesthetic technique. Otolaryngol Head Neck Surg. 201; 148: 548-556.
- Ahn D, Sohn JH, Lee GJ. Feasibility of a new V-shaped incision for parotidectomy: a preliminary report. Br J Oral Maxillofac Surg. 2018; 56: 406-410
- Jo MG, Lee DJ, Cha W. A modified V-shaped incision combined with superficial musculo-aponeurotic system flap for parotidectomy. Acta Otolaryngol. 2019; 139:178-183
- Zhang Q, Yang Y, Yang P, Tan Y, Liu X, Xiong B, et al. Cosmetic approach selection in parotidectomy for benign parotid gland tumour according to its location. J Plast Reconstr Aesthet Surg. 2020; 73: 921-926
- Kim DY, Park GC, Cho YW, Choi SH. Partial Superficial Parotidectomy via Retroauricular Hairline Incision. Clin Exp Otorhinolaryngol. 2014; 7: 119-22
- Ahn D, Lee GJ, Sohn JH. Individualized Use of Facelift, Retroauricular Hairline, and V-Shaped Incisions for Parotidectomy. J Oral Maxillofac Surg. 2020; 78: 2339.
- Yuen AP. Small access postaural parotidectomy: an analysis of techniques, feasibility and safety. Eur Arch Otorhinolaryngol. 2016; 273: 1879-1883.
- Moori PL, Rahman S. Endoscopic versus conventional parotid gland excision: a systematic review and meta-analysis. Br J Oral Maxillofac Surg. 2021; 59: 272-280.
- Yen TL, Driscoll CL, Lalwani AK. Significance of House-Brackmann facial nerve grading global score in the setting of differential facial nerve function. Otol Neurotol. 2003; 24: 118-22
- Quer M, Vander Poorten V, Takes RP, Silver CE, Boedeker CC, de Bree R, et al. Surgical options in benign parotid tumors: a proposal for classification. Eur Arch Otorhinolaryngol. 2017; 274: 3825-3836
- Aggarwal V. Incisions for Parotidectomy: A Narrative Review. Ann Plast Surg. 2021; 87: e71-e78
- Stathopoulos P, Igoumenakis D, Smith WP. Partial Superficial, Superficial, and Total Parotidectomy in the Management of Benign Parotid Gland Tumors: A 10-Year Prospective Study of 205 Patients. J Oral Maxillofac Surg. 2018; 76: 455-459
- Chiesa-Estomba CM, Larruscain-Sarasola E, Lechien JR, Mouawad F, Calvo-Henriquez C, Diom ES, et al. Facial nerve monitoring during parotid gland surgery: a systematic review and meta-analysis. Eur Arch Otorhinolaryngol. 2021; 278: 933-943