Identification and Management of Glottic Closures in Patients with Bulbar Weakness Amyotrophic Lateral Sclerosis Requiring Noninvasive Ventilation
- #. These authors have contributed equally to the work and share first authorship
- 1. Department of Medicine, University of Texas Southwestern Medical Center, USA
Abstract
Noninvasive ventilation has become standard-of-care management for patients with amyotrophic lateral sclerosis (ALS) but remains a challenging intervention for patients with bulbar weakness. Noninvasive ventilation can itself trigger sleep-disordered breathing events in the form of glottic closure, which can limit success of the intervention. Complexity arises from impaired airway clearance, secretion management, and positive pressure related airway collapse. This review highlights the approach to identification and management of glottic closure and airway complications associated with noninvasive ventilation in patients with bulbar weakness secondary to ALS.
Keywords
• Airway
• Amyotrophic Lateral Sclerosis
• Bulbar Weakness
• Glottic Closure
• Laryngospasm
• Sialorrhea
• Noninvasive Ventilation
Citation
Krishnan G, Dula M, Lussier BL (2026) Identification and Management of Glottic Closures in Patients with Bulbar Weakness Amyotrophic Lateral Sclerosis Requiring Noninvasive Ventilation. Ann Otolaryngol Rhinol 13(1): 1379.
INTRODUCTION
Amyotrophic lateral sclerosis (ALS) and motor neuron disease is characterized by loss of motor neurons in the cortex, brainstem and spinal cord resulting in progressive weakness of the limbs, respiratory and bulbar muscles leading to death from respiratory failure in the majority of patients. Nearly all patients develop bulbar symptoms with disease progression, either early or late in the disease process depending on site of onset. Symptoms attributable to lower motor neuron failure (true bulbar palsy) or upper motor neuron weakness (pseudobulbar palsy) include dysarthria, dysphagia, difficulty managing oropharyngeal secretions and impaired cough can be accompanied by significant glottic dysfunction and laryngospasm [1].
Glottic closure during noninvasive ventilation (NIV) is a dynamic obstruction at the level of the vocal cords, typically a triggered laryngeal closure that impedes airflow and reduces the efficacy of NIV. This phenomenon may be mediated by bronchopulmonary receptors, laryngospasm or vocal cord paralysis, or in the case of neuromuscular disease, a combination of factors [2,3].
This article will focus specifically on the management of the airway and glottic closures during noninvasive ventilation, particularly those precipitated by excess ventilatory support / turbulent breath delivery during NIV and pooling of oropharyngeal secretions.
IDENTIFYING GLOTTIC CLOSURES
Identification of glottic closures is challenging as direct videolaryngoscopy in real-time to assess glottic movement and identify the mechanism of airflow limitation during for discontinuous glottic closures is challenging [2-4]. Adjunct monitoring has been used to monitor efficacy of NIV in the acute and home setting, and may be used to augment detection of glottic closures precipitated by NIV [5,6]. Typically, these occur with Waveform capnography is also technically challenging during NIV, and the sensitivity of transcutaneous monitoring may be insufficient to detect rapid glottic closure on a breath-to-breath basis.
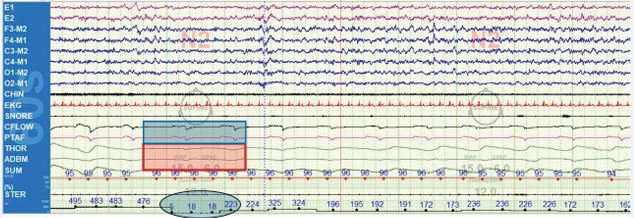
Polysomnographic features of glottic closures are often subtle and easily mistaken for obstructive or hypopneic events. Findings may appear as reduced or absent thoracic or abdominal excursion with machine-delivered breaths, or a marked reduction in exhaled volume following a machine-triggered breath without abdominal or thoracic excursion (Figure 1). There may or may not be a hypoxic event that meets hypopneic or apneic criteria and thus may be overlooked. Similarly, this is typically noted in N2 or REM sleep and may be associated with subsequent hyperventilation and a resulting lowering of carbon dioxide [7]. With experience and a high index of suspicion, use of end-tidal or transcutaneous carbon dioxide and pulse oximetry monitoring during polysomnography can be used to correlate dyssynchronous (or failed) breath delivery with patient effort and differentiate from obstructive apnea in real-time during noninvasive ventilation. In this way, polysomnography during NIV titration may be used guide individualized modification to ventilatory support [6].
Figure 1 Example of glottic closure noted on polysomnography with titration of noninvasive ventilation. This is a 60 second epoch from a polysomnogram for a 52-year-old woman with progressive bulbar weakness secondary to amyotrophic lateral sclerosis. Evident are the machine-delivered breathes (blue box) based on timing of delivery with no significant abdominal or thoracic excursion (red box) and a loss of exhaled tidal volume (circled). Note there is no significant detectable desaturation during these transient events.
Review of remote monitoring data available through commercially available home NIV devices may show increasing apneic or hypopneic events during use and may be clinically correlated with self-reported secretion volume, and changes in breath delivery characteristics including rise, inspiratory pressure, or expiratory positive airway pressure (EPAP) over time. Clinically, if the patient is aware of precipitated glottic closures, the sensation of choking at the time of breath delivery is most informative and may prompt changes in approach to NIV.
MODIFYING NIV FOR PATIENTS WITH NIV
Management strategies focus on identification of precipitants, particularly secretions in patients with sialorrhea, and adjustments to ventilation to minimize turbulent flow. There is limited evidence to support a specific strategy but optimizing interface and reducing unanticipated or rapid changes or turbulence in airflow are the primary interventions.Switching from an oronasal interface to a nasal mask may limit the turbulence of airflow that reaches the oropharynx/laryngopharynx [7-11].
The speed at which the breath, particularly an unanticipated breath delivered via a backup rate triggered by elapsed time rather than patient-trigger, have been implicated in glottic closure and subjective dysynchrony. Glottic closures appear to abate with reduction in rise (speed of inspiratory pressure) and reducing the set back-up respiratory rate to allow preferentially patient triggered breaths. Similarly, unanticipated auto-triggering may be a significant precipitant, particularly in patients with a very sensitive trigger setting who have a high volume of secretions, and the trigger sensitivity may require adjustment [7-11].
Debate exists over increasing EPAP to overcome airflow limitation or reduction in EPAP as a precipitant. Some evidence supports higher EPAP, as delivered by high-flow nasal cannula may be better than low EPAP, though there are no comparison studies that adjust for heat, humidification, and flow delivery at the level of the larynx to prevent laryngospasm. The general approach to ventilatory support in chronic neuromuscular disease is to titrate inspiratory support to ensure ventilation and apply the lowest EPAP sufficient to overcome sleep related obstructive apnea, minimizing EPAP for any daytime needs to allow for function. In theory, higher EPAP may be associated with a positive intrathoracic pressure, which has been shown to inhibit glottic closure and laryngospasm [12]. The counterargument is that even low EPAP is sufficient to prevent negative intrathoracic pressure precipitating glottic closures, particularly with sufficient inspiratory support. Further, up-titration of EPAP has been associated with retained secretions and increased events attributable to glottic closures (Figure 1). While further evidence is required to guide one strategy over another, titration of EPAP may be an important approach to ventilation management if glottic closures are identified. This is an especially important consideration given the increase in utilization of auto titrating features on home NIV devices. The auto-titration algorithms respond to airflow limitations as obstructions independent of patient efforts and rapid changes in EPAP over a wide prescription range may have deleterious effects. The authors recommend caution allowing wide ranges of auto-titrating EPAP features for patients at risk for NIV precipitant glottic closures.
There are no published protocols to monitor or guide titration of ventilation adjustments or interface selection for glottic closures in the acute care or outpatient setting, highlighting the need for further research in this area (Table 1).
Table 1: Summary of glottic closure characteristics and mitigation strategy. Note the difference in polysomnographic features from obstructive sleep apnea, during which there would be abdominal/ thoracic efforts that does not lead to machine delivery of support. N2= stage N2 sleep; EPAP = expiratory positive airway pressure.
|
Clinical symptoms |
Polysomnographic Features |
Precipitant mechanism |
Mitigation approach [7-11] |
|
Poor sleep quality Sensation of choking with air delivery |
Machine delivered-breath associated with reduced or absent thoracic/ abdominal excursion drop in exhaled volumes relative to spontaneous breathes Predominantly in N2 sleep May be associated with hyperventilation |
Excess ventilatory support Turbulent airflow |
Heated humidification of circuit Trial of nasal interface Reduce the backup respiratory rate Reduce / slow breath rise Reduce pressure support to normalize CO2 if there is concern for precipitant central apnea Increase EPAP / Decrease EPAP if high and reassess |
|
Aspiration of secretions with appropriate glottic closure reflex |
Anti-sialagogues Nasal interface to prevent pooling Reducing gastrointestinal reflux Escalate airway clearance measures |
||
|
Exaggerated glottic closure reflex / laryngospasm |
Muscle relaxants may be considered, though limited evidence to support long-term |
AIRWAY CLEARANCE
Success of noninvasive ventilation depends on patency of the upper airway and thus limited if airway clearance is not optimized. Similar to the challenges using positive pressure NIV in patients with bulbar weakness, positive pressure insufflation employed in airway clearance as part of standard care may be complicated by glottic closure / laryngospasm. Parallels may be drawn between approach to airway clearance and noninvasive ventilation, and patients with bulbar weakness typically require tailoring of both techniques simultaneously.
ANTISIALAGOGUES
Sialorrhea is a common symptom in amyotrophic lateral sclerosis (ALS) patients due to impaired ability to effectively swallow and clear saliva from bulbar dysfunction. Fifty percent of patients with ALS experience problems handling serous saliva and 20% fail to achieve adequate control of sialorrhea [13]. In addition to the significant negative impact on quality of life with social embarrassment from drooling and psychological stress, patients live in realistic fear of life-threatening aspiration. Post-mortem studies show aspiration pneumonia as the primary cause of death in 20% of ALS patients, with an additional 11% of deaths stemming from a combination of aspiration pneumonia and bronchopneumonia [14]. NIV is less effective and/or poorly tolerated in patients with poorly controlled sialorrhea. While laryngospasm and glottic closure is reported in relation to both bolus aspiration and pooling of secretions [1], and complications to bulbar dysfunction, micro-aspiration and subclinical glottic closures during NIV are chronic and underreported phenomenon and potentially contribute to long term outcomes. Therefore, guided management with various pharmacologic and non-pharmacologic strategies for treating sialorrhea in ALS should be considered.
Anticholinergics (e.g., glycopyrrolate, sublingual atropine or hyoscyamine, scopolamine) are widely used as a “first-line” treatment for sialorrhea in ALS due to ease of administration and less invasive than other options such as botulinum toxin injections or radiotherapy. These medications act as antisialogogues by preventing acetylcholine from activating muscarinic receptors on the salivary glands, thus resulting in a reduction in the amount of saliva production. Amitriptyline, a tricyclic antidepressant used to treat comorbid sleep disruption, pain and emotional lability, has some anticholinergic properties and may help control excess secretions in ALS patients. The American College of Chest Physicians recommends a therapeutic trial of anticholinergics with consideration for continued use only if benefits outweigh the side effects of dry mouth, constipation, cognitive impairment, and urinary retention [6]. The national ALS Patient CARE database indicates that more than half of ALS patients responded to treatment with atropine, glycopyrrolate, or amitriptyline [15].
In refractory cases where oral and transdermal pharmacologic treatments have been ineffective or poorly tolerated, botulinum toxin injections and radiotherapy are recognized as suitable alternatives. Botulinum neurotoxin type A (BoNT-A) or B (BoNT-A) is typically injected to both the parotid glands and submandibular glands under ultrasound guidance to inhibit acetylcholine release at presynaptic nerve terminals to reduce salivary secretion. Multiple randomized controlled trials show similar results between the two types in benefit duration between 75 90 days with BoNT-B having a shorter latency [16]. The potential for rapid progression of dysphagia following botulinum toxin injection should be considered when treating patients who are still eating for pleasure or dependent on oral route for nutritional support.
Radiation therapy (RT) offers another longer-term benefit after anticholinergic agents and botulinum toxin injections have been unsuccessful. Low-dose radiation to the bilateral submandibular glands and whole or partial bilateral parotid glands are targeted to reduce saliva production by causing damage and fibrosis to the secretory epithelial cells. The response to RT provides symptom relief for up to 6 months with a relatively low probability for radiation-induced malignancy since it takes a decade or longer to develop following RT [17]. The most common adverse effect is the intentional xerostomia which is at times severe.
MUSCLE RELAXANTS
No studies have evaluated the effect of antispasmodic agents on glottic closures and tolerance of NIV. There are small case series trialing baclofen and diazepam for precipitated glottic closure, laryngeal dystonia, or fixed asymmetric dystonia in supranuclear palsy [18,19].
COUGH AUGMENTATION AND AIRWAY CLEARANCE
In patients with ALS complicated by bulbar dysfunction resulting in glottic closure, airway clearance is a major challenge as loss of glottic control limits results in buildup of backpressure to generate peak cough flows sufficient to clear secretions. Many standard airway clearance strategies such as vibration vests and oscillatory PEP devices (e.g., Acapella, Flutter) have limited utility in this patient population, since they rely on intact respiratory muscle and glottic coordination to move secretions proximally. Consequently, they are generally ineffective and often counterproductive in neuromuscular disease. These vibratory techniques can increase upper airway turbulence and stimulate reflex glottic closure, worsening secretion retention. Instead, a cough assist device allowing for mechanical insufflation–exsufflation (MI-E) is the preferred modality. MI-E bypasses the need for voluntary glottic control and generates an artificial cough by rapidly cycling between positive and negative pressures, simulating the inspiratory and expiratory phases of a normal cough [20,21].
For patients with ALS and glottic closure, the key to successful MI-E lies in pressure and rise-time adjustments. High insufflation pressures delivered too quickly can again provoke reflex closure of the vocal cords [21]. To minimize this, the authors recommend titration of MIE devices with a slower rise time (gentler pressure ramp; 400-800ms) and moderate pressures (for example, +30 to +35 cm H?O for insufflation and –35 to –40 cm H?O for exsufflation). Once the patient tolerates slower insufflation without upper airway closure, pressures can be gradually increased (+40/–40 cm H?O or higher) to optimize peak cough flow (>160 L/min goal for secretion clearance).
Manual or high-frequency chest wall oscillation is also a consideration in these patients. These modalities may help mobilize distal mucus, but they still cannot substitute for an effective expulsive phase; without sufficient cough flow, secretions mobilize distally and pool centrally. Thus, in ALS with bulbar dysfunction, MI-E remains the cornerstone of airway clearance [20].
Andersen et al. explored laryngeal and upper airway response patterns to insufflation-exsufflation in patients with bulbar ALS, commonly employed as standard airway clearance and lung volume recruitment in patients with progressive neuromuscular disease. These efforts identified that patients with hypotonic bulbar weakness and patients with spastic pseudobulbar features both tended to have exaggerated constriction of hypopharynx during exsufflation, though much more pronounced in the patient’s hypotonic bulbar weakness. Additionally, insufflation specifically caused adduction of aryepiglottic folds at insufflation pressures of 20-50 cm H2 O, and at higher pressures both the aryepiglottic folds and true vocal cords closed during insufflation on patients with pseudobulbar palsy [22]. While insufflation pressures are typically stronger with a much faster rise than NIV pressures used for chronic ventilatory support, there is a parallel to consider in risk assessment.
SUMMARY
Patients who tolerate NIV have a longer survival than those who are unable to tolerate, and of the groups that tolerate NIV, it is typically those with a higher FVC and fewer bulbar symptoms [5-24]. Understanding the pathology to allow careful titration of settings may improve the tolerance of NIV. Upper airway reflexes may predispose patients undergoing NIV to laryngospasm and glottic closures, either clinical or subclinical, related to aspiration of secretions or turbulent airflow. Risk stratification based on pseudobulbar palsy or hypotonic bulbar palsy and tolerance of insufflation and exsufflation may help identify patients at highest risk for glottic closures. Careful clinical assessment potentially augmented by polysomnography or careful review of downloaded device data may identify patients developing recurrent glottic closure so measures can be taken to mitigate the complication. It is of utmost importance that glottic closures be addressed via secretion control or tailored NIV modification before deeming NIV a futile intervention for a particular patient.
AUTHOR CONTRIBUTIONS
G Krishnan: writing, review, editing. M. Dula: writing, review, editing; B. Lussier: conceptualization, writing, review, editing.
REFERENCES
- Simonds AK. Progress in respiratory management of bulbar complications of motor neuron disease/amyotrophic lateral sclerosis? Thorax. 2017; 72: 199-201.
- Oppersma E, Doorduin J, Gooskens PJ, Roesthuis LH, van der Heijden EHFM, van der Hoeven JG, et al. Glottic patency during noninvasive ventilation in patients with chronic obstructive pulmonary disease. Respir Physiol Neurobiol. 2019; 259: 53-57.
- Roy B, Samson N, Moreau-Bussière F, Ouimet A, Dorion D, Mayer S, et al. Mechanisms of active laryngeal closure during noninvasive intermittent positive pressure ventilation in nonsedated lambs. J Appl Physiol (1985). 2008; 105: 1406-1412.
- Sayas Catalán J, Jiménez Huerta I, Benavides Mañas P, Luján M, López- Padilla D, Arias Arias E, et al. Videolaryngoscopy With Noninvasive Ventilation in Subjects With Upper-Airway Obstruction. Respir Care. 2017; 62: 222-230.
- Aboussouan LS, Khan SU, Meeker DP, Stelmach K, Mitsumoto H. Effect of noninvasive positive-pressure ventilation on survival in amyotrophic lateral sclerosis. Ann Intern Med. 1997; 127: 450-453.
- Khan A, Frazer-Green L, Amin R, Wolfe L, Faulkner G, Casey K, et al. Respiratory Management of Patients With Neuromuscular Weakness: An American College of Chest Physicians Clinical Practice Guideline and Expert Panel Report. Chest. 2023; 164: 394-413.
- Aboussouan LS. Sleep-disordered Breathing in Neuromuscular
- Jounieaux V, Aubert G, Dury M, Delguste P, Rodenstein DO. Effects of nasal positive-pressure hyperventilation on the glottis in normal sleeping subjects. J Appl Physiol (1985). 1995; 79: 186-193.
- Parreira VF, Delguste P, Jounieaux V, Aubert G, Dury M, Rodenstein DO. Glottic aperture and effective minute ventilation during nasal two-level positive pressure ventilation in spontaneous mode. Am J Respir Crit Care Med. 1996; 154: 1857-1863.
- Parreira VF, Jounieaux V, Aubert G, Dury M, Delguste PE, Rodenstein DO. Nasal two-level positive-pressure ventilation in normal subjects. Effects of the glottis and ventilation. Am J Respir Crit Care Med. 1996; 153: 1616-1623.
- Ikari T, Sasaki CT. Glottic closure reflex: control mechanisms. Ann Otol Rhinol Laryngol. 1980; 89: 220-224.
- Stone CA, O’Leary N. Systematic review of the effectiveness of botulinum toxin or radiotherapy for sialorrhea in patients with amyotrophic lateral sclerosis. J Pain Symptom Manag. 2009; 37: 246- 258.
- Burkhardt C, Neuwirth C, Sommacal A, Andersen PM, Weber M. Is survival improved by the use of NIV and PEG in amyotrophic lateral sclerosis (ALS)? A post-mortem study of 80 ALS patients. PLoS One. 2017; 12: e0177555.
- Garuti G, Rao F, Ribuffo V, Sansone VA. Sialorrhea in patients with ALS: current treatment options. Degener Neurol Neuromuscul Dis. 2019; 9: 19-26.
- Guidubaldi A, Fasano A, Ialongo T, Piano C, Pompili M, Mascianà R, et al. Botulinum toxin A versus B in sialorrhea: a prospective, randomized, double-blind, crossover pilot study in patients with amyotrophic lateral sclerosis or Parkinson’s disease. Mov Disord. 2011; 26: 313-319.
- Slade A, Stanic S. Managing excessive saliva with salivary gland irradiation in patients with amyotrophic lateral sclerosis. J Neurol Sci. 2015; 352: 34-36.
- Blitzer A, Brin MF, Stewart CF. Botulinum toxin management of spasmodic dysphonia (laryngeal dystonia): a 12-year experience in more than 900 patients. Laryngoscope. 1998; 108: 1435-1441.
- Brin MF, Blitzer A, Stewart C. Laryngeal dystonia (spasmodic dysphonia): observations of 901 patients and treatment with botulinum toxin. Adv Neurol. 1998; 78: 237-252.
- Chatwin M, Toussaint M, Gonçalves MR, Sheers N, Mellies U, Gonzales- Bermejo J, et al. Airway clearance techniques in neuromuscular disorders: A state of the art review. Respir Med. 2018; 136: 98-110.
- Shah NM, Apps C, Kaltsakas G, Madden-Scott S, Suh ES, D’Cruz RF, et al. The Effect of Pressure Changes During Mechanical Insufflation- Exsufflation on Respiratory and Airway Physiology. Chest. 2024; 165: 929-941.
- Andersen T, Sandnes A, Brekka AK, Hilland M, Clemm H, Fondenes O, et al. Laryngeal response patterns influence the efficacy of mechanical assisted cough in amyotrophic lateral sclerosis. Thorax. 2017; 72: 221-229.
- Bourke SC, Tomlinson M, Williams TL, Bullock RE, Shaw PJ, Gibson GJ. Effects of non-invasive ventilation on survival and quality of life in patients with amyotrophic lateral sclerosis: a randomised controlled trial. Lancet Neurol. 2006; 5: 140-147.
- Farrero E, Prats E, Povedano M, Martinez-Matos JA, Manresa F, Escarrabill J. Survival in amyotrophic lateral sclerosis with home mechanical ventilation: the impact of systematic respiratory assessment and bulbar involvement. Chest. 2005; 127: 2132-2138.