Otitis Media and Ventilation Tube Insertion and Quality of Life in a Rural Population in Denmark – Data from the LOFUS Cohort
- 1. Department of Otorhinolaryngology and Maxillofacial Surgery, Zealand University Hospital, Denmark
- 2. Department of Clinical Medicine, University of Copenhagen, Denmark
Abstract
Background: Otitis media (OM) is among the most common infections in childhood. Approximately 60% of all children will experience one or more episodes of OM before the age of 7, and 26% of children in Denmark are treated with Ventilation Tube Insertion (VTI) before the age of 7. Previous studies investigating the effects of VTI on quality of life (QoL) for children and caregivers have yielded conflicting results. Here, we investigate whether OM and VTI affect the QoL in children and their families in rural setting of Denmark.
Methods: From the LOFUS cohort, caregivers of 1.169 children aged 2-10 years, answered questions on how OM affects the children’s and their family’s general QoL. Additionally, we used Visual Analogue Scales from zero (no effect) to 10 (worst possible effect) to score the impact on QoL.
Results: In 480 children (43%) were not reported any episodes of OM, 385 (35%) children had 1-3 episodes and 247 (22%) children had >3 episodes. Twenty-six percent of the total childhood cohort and 47% of children who reported OM had had VTI procedure performed. We found an Odds Ratio (OR) of 1.54 (0.36-10.62) and 2.66 (0.62-18.41) for poorer QoL in the affected child and an OR of 1.13 (0.26-7.91) and 1.91 (0.43-13.34) for poorer QoL in the family, for 1-3 and >3 episodes, respectively. VTI yielded an OR of 2.13 (95% CI 1.48-3.08, p<0.001) and 2.27 (95% CI 1.54-3.37, p<0.001) for poorer QoL on children’s and family’s QoL, respectively.
Conclusion: Our study shows a high frequency of reported OM and a high frequency of VTI procedures performed in a rural population in Denmark. Furthermore, the study shows an association correlation between VTI and poorer QoL in the children and in their families.
Keywords
• Otitis Media
• Ventilation tube insertion
• Questionnaire survey
• OM-6
• Quality Of Life
• LOFUS Metrics
Citation
Søborg T, Kørvel-Hanquist A, Homøe P (2024) Otitis Media and Ventilation Tube Insertion and Quality of Life in a Rural Population in Denmark – Data from the LOFUS Cohort. Ann Otolaryngol Rhinol 11(5): 1346.
INTRODUCTION
Otitis media (OM) is among the most common infections in childhood [1]. Approximately 60% of all children will experience one or more episodes of OM before the age of 7, and 26% of children in Denmark have been treated with Ventilation Tube Insertion (VTI) before the age of 7 [1]. In Denmark, approximately 55.000 children are treated with VTI annually, demonstrating the highest incidence of VTI insertions reported worldwide with a continuing increase [2]. In Denmark the hospitals account for 4% of the procedures and the private ENT-clinics for 96% [2]. The worldwide socioeconomic consequences of OM are substantial, primarily from treatment and management of the disease and parental absence from work [3,4]. OM is subcategorized in three forms: Acute OM (AOM), an acute inflammation caused by viral or bacterial infections, OM with Effusion (OME), which is accumulation of fluid in the middle ear without acute symptoms, and if it persists for a minimum of three months is referred to as Chronic OME (COME). Children suffering from OM present with varied symptomatology largely depending on age of onset. The most frequent symptom in older children is a history of rapid onset ear pain. However, in young preverbal children, otalgia as suggested by tugging/rubbing/holding of the ear, excessive crying, fever, or changes in the child’s sleep or behavioral patterns are the most frequent symptoms. The prevalence of AOM peaks at the age of 6-18 months [1]. Recurrent AOM (rAOM) is defined by experiencing three or more episodes of AOM in six months or four episodes in one year with interludial periods of remission [5] and can be a great strain on both the child and the family. OM is often associated with upper respiratory tract infections and known risk factors for OM comprise: living together with older siblings, early daycare attendance, early termination of breastfeeding, passive smoking and crowded households [6]. The incidence of OM has been growing in western countries for decades, and the reason for this is thought to be an increase in use of day care institutions [7]. Tympanostomy tubes are used for treatment of COME but also rAOM as an alternative to longterm or recurrent antibiotic courses [8,9]. The impact of OM on children’s and their families Quality Of Life (QoL) have only been sparsely investigated and previous studies investigating the effects of VTI on QoL for children and caregivers have yielded conflicting results [10-15]. Here, we investigate whether OM and VTI affect the QoL in children and families living in rural Denmark using population-based data obtained from The Lolland-Falster Health Study (LOFUS) cohort.
What This Study Adds
This study adds to knowledge concerning how OM affects QoL in rural Danish families by use of the population-based LOFUS cohort questionnaire [16]. Also, the study adds to the knowledge concerning the affect on QoL of VTI in children, in their family.
MATERIAL AND METHODS
Study Design
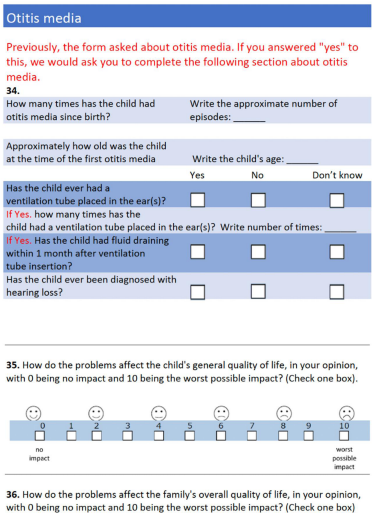
The study was conducted as a cross-sectional populationbased questionnaire survey. The LOFUS questionnaires were constructed from a combination of previously used items and scales as well as new purpose-developed scales [17] including four of the questions from a modified version of the Danish validated OM-6 questionnaire [18]. The OM-6 questions that were excluded in the questionnaire were ‘Activity Limitations’ and ‘Caregiver Concerns’. This approach was due to administrative limitations on number of total questions in the comprehensive overall LOFUS questionnaire. The participants were encouraged to complete their questionnaires electronically at home prior to a physical examination, but, if needed, they could get help from staff after the physical examination. Paper-based versions were used only if participants could not master the electronic questionnaires. The possibility of audio-computer aided response was not possible. Five, partially different, questionnaires were used for the age groups 0-1, 2-3, 4-10, 11-17, and >18 years. Caregivers were instructed to complete the questionnaire for children aged <10 years. The specific questions concerning OM and QoL including the applied VAS scale are shown translated to English in Appendix 1.
Study Population
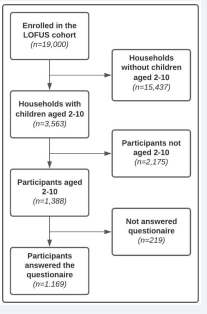
LOFUS is a publicly funded population survey conducted in the two remote municipalities of Lolland and Guldborgsund, located in a socio-economically disadvantaged area of Denmark roughly 140 km south of the capital Copenhagen. In the 2020 national ranking of all 98 municipalities, these two were ranked as the last and the sixth last municipalities measured by socioeconomic index [19]. Together, the municipalities comprise 103.000 citizens. Participants were randomly selected by civil registration number, invited by mail, and re-invited by phone. The LOFUS study covers several health areas: mental health, health literacy, social issues, genetics, kidney, ear nose & throat problems and more. Beyond questionnaire responses, LOFUS data contains blood samples and biometrics. From February 2016 to February 2020, 19.000 people, aged 0-96, participated in the LOFUS and filled out the questionnaires. LOFUS is described in detail elsewhere [16]. The focus for the present study was on children aged 2-10 years of age. In the LOFUS cohort a total of 1,388 children were aged 2-10 [Figure 1]. A total of 1,169 parents answered questions concerning OM, VTI and QoL. BMI was calculated in 1,338 children where both weight and height were provided. BMI was predominantly normal for all ages (at least 77%), and the prevalence of overweight was 13%, while the prevalence of obesity was 5%. Parents answering the questionnaire were more likely to be married/in partnership (95%) than divorced, widow(er) or single, had a vocational or shorter higher education (48%) than no, medium, or long higher education and employed (incl. self-employed) (87%) than student or out of work. The distribution of girls and boys were 574 and 595, respectively (49% vs. 51%) [Table 1].
Table 1: Civil status, education level and occupation status of answering parents
|
Gender |
n |
% |
|
Female |
710 |
57 |
|
Male |
532 |
43 |
|
Civil status |
|
|
|
Married/partnership |
1176 |
95 |
|
Divorced/widow(er)/single |
63 |
5 |
|
Highest Education |
|
|
|
One or multiple shorter courses/no formal education/other |
151 |
12 |
|
Vocational or shorter higher education |
592 |
48 |
|
Medium or long higher education |
496 |
40 |
|
Occupation |
|
|
|
Employed (incl. self-employed) |
1078 |
87 |
|
Student |
53 |
4 |
|
Out of work (Unemployed/Retired early/social benefit) |
111 |
9 |
Figure 1 Diagram showing the intended participants in the LOFUS cohort and the enrolled participants in the present study.
Data selection
The inclusion criteria were response from caregivers of children aged 2 to 10 and the exclusion criteria were failure to answer scales on OM affecting QoL in the child and the family along with questions concerning if the child have had OM and VTI. Civil status, highest education and occupational status of the parents were also collected along with relevant medical information on the children.
Main outcome measures
The questionnaire specific for OM, included eight questions for all age groups including if the child has had OM (see appendix). The main outcomes were the answers to the two questions on how OM affects the children’s general QoL as well as the families QoL. The QoL assessment was presented on a Visual Analogue Scale (VAS) from zero (no affect of disease on QoL) to 10 (worst possible affect on QoL). An additional page of the modified OM-6 questionnaire including the items, impact on physical suffering, hearing loss, speech impairment and emotional distress was answered if the child had had episodes of OM. Answers of the modified OM-6 questionnaire were scaled from 1 to 7, and the mark 1 was “not present/not a problem” and 7 was “extremely high impact”. Means for the four chosen items of the modified OM-6 questionnaire including VAS on children who have had VTI and no VTI were tested for differences. We stratified episodes of OM in the groups 0, 1-3 and >3 and of those who had OM whether they had VTI or not. Except for number of remembered OM episodes, we did not have information on other aspects e.g., exact age of the children when having the OM episodes. Also, as this is a questionnaire survey, we did not have information on the time between OM episodes or VTI placement and completion of the questionnaire or how and where the VTI was performed.
Appendix (Questions and VAS scales regarding otitis media translated to English)
Secondary outcomes were co-variables as allergy/hay fever, asthma/asthmatic bronchitis, atopic dermatitis and living with siblings. These were tested for correlation to child and family QoL. As Body Mass Index (BMI) is known to be a proxy parameter for socio-economic differences [20,21], we also tested the association between BMI against OM and VTI. BMI was estimated for each age group using ‘Body mass index-for-age percentile growth chart’ sheets from Center of Disease Control and Prevention (CDC) [22]. The values were read as mean value for each age. Normal weight is from the 5th up to the 85th percentile. Further, underweight is less than the 5th percentile, overweight from 85th percentile. Further, underweight is less than the 5th percentile, overweight from 85th to less than the 95th percentile and obesity is ≥ 95th percentile.
Statistical methods
Descriptive statistics are presented as count values and percentages as well as means withs 95% confidence intervals unless otherwise indicated. Data on the 11-point QoL scale in children who had one or more OM were divided into four groups: ‘No effect’, ‘mild’, ‘moderate’ and ‘severe’ from the values 0, 1-3, 4-6 and 7-10 to increase the numbers in the groups. The main outcome parameters, i.e., effect on QoL on a Likert scale, as well as covariables were investigated with ordinal logistic regression to account for the hierarchical structure of the categories on the scale. The results are presented as Odds Ratios (ORs) and 95% Confidence Intervals (CIs). Correlation between BMI and OM/VTI was assessed by logistic regression and presented by p-values. Differences in means of the modified OM-6 questionnaire were assessed by t-test. A p-value of less than 0.05 was considered statistically significant. All analyses were performed in R version 4.0.5.
Approvals and registrations
This study has been approved by The Danish Data Protection Agency (REG-014-2021). Region Zealand’s Ethical Committee on Health Research (SJ421) and The Danish Data Protection Agency (REG-24-2015) approved the LOFUS study. The LOFUS study is registered in ClinicalTrials.gov (NCT02482896) [16].
RESULTS
In total, 57% of all children were reported to have had at least one episode of OM. Of those, 35% were in the 1-3 OM group and 22% reported >3 episodes of OM. Three hundred one (26% of the children in the cohort had been treated with VTI and 47% of the children who had had one or more OM) had been treated with VTI [Table 2]. Average episodes of OM in children with no VTI vs. children with VTI were 2.37 vs. 4.33, respectively.
Table 2: Demographic and Descriptive Data of the Total Sample of included children
|
|
2-3 years |
4-6 years |
7-10 years |
|||
|
Gender |
n |
% |
n |
% |
n |
% |
|
Girls |
110 |
(57) |
173 |
(48) |
291 |
(47) |
|
Boys |
83 |
(43) |
190 |
(52) |
322 |
(53) |
|
BMI |
|
|
|
|
|
|
|
Underweight |
14 |
(7) |
32 |
(7) |
64 |
(9) |
|
Normal weight |
178 |
(84) |
344 |
(81) |
539 |
(77) |
|
Overweight |
15 |
(7) |
33 |
(8) |
56 |
(8) |
|
Obese |
5 |
(2) |
16 |
(4) |
42 |
(6) |
|
Siblings* |
|
|
|
|
|
|
|
0 |
43 |
(22) |
49 |
(14) |
99 |
(16) |
|
1 |
102 |
(53) |
204 |
(56) |
313 |
(51) |
|
2 |
40 |
(21) |
84 |
(23) |
157 |
(26) |
|
3 |
8 |
(4) |
21 |
(6) |
42 |
(7) |
|
4 |
|
|
5 |
(1) |
1 |
(<1) |
|
6 |
|
|
|
|
1 |
(<1) |
|
No. of OM |
|
|
|
|
|
|
|
0 |
92 |
(49) |
154 |
(44) |
234 |
(41) |
|
1-3 |
64 |
(34) |
118 |
(34) |
203 |
(35) |
|
>3 |
32 |
(17) |
75 |
(22) |
140 |
(24) |
|
VTI |
|
|
|
|
|
|
|
Yes |
42 |
(44) |
105 |
(53) |
154 |
(44) |
|
No |
54 |
(56) |
93 |
(47) |
199 |
(56) |
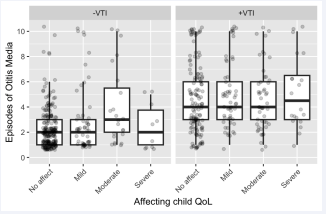
Figure 2 Showing number of otitis media episodes and categories of QoL scores in the children according to ventilation tube insertion (VTI) or no VTI.
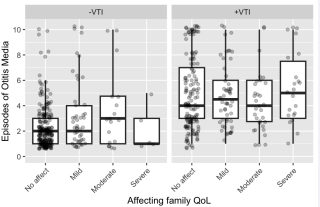
Figure 3 Showing number of otitis media episodes and categories of QoL scores i
Main outcome: The affect of QoL in child and family are illustrated in Figure 2 and 3. We found an OR of 1.54 and an OR of 2.66 for being placed in a poorer child QoL category and an OR of 1.13 and an OR of 1.91 for poorer family QoL, respectively. All OR’s were non-significant [Table 3]. Children who had had VTI had an OR of 2.13 (p<0.001) and 2.27 (p<0.001) for being placed in a poorer QoL category on child and family QoL, respectively [Table 3].
Table 3: Effect of reported numbers of otitis media (OM) and reported ventilation tube inse.
|
|
QoL child* |
QoL family* |
||||
|
|
OR |
95% CI |
p-value |
OR |
95% CI |
p-value |
|
1-3 OM |
1.54 |
0.36-10.62 |
0.600 |
1.13 |
0.26-7.91 |
0.880 |
|
>3 OM |
2.66 |
0.62-18.41 |
0.234 |
1.91 |
0.43-13.34 |
0.437 |
|
VTI |
2.13 |
1.48-3.08 |
<0.001 |
2.27 |
1.54-3.37 |
<0.001 |
For the means of the four items of the modified OM-6 questionnaire and the means of the VAS-scale QoL measures we found that children who had VTI scored significantly worse except for physical suffering compared to children with no VTI [Table 4]. Previous studies have shown association between lower socioeconomic status and high BMI in children [20,21]. Also, other studies have shown association between childhood obesity and OM [23]. We found no correlation between BMI and OM but an association between the BMI subcategory “overweight” and VTI (not shown). Finally, we found no association on QoL of relevant co-variables [Table 5].
Table 4: Mean results of a modified OM-6 questionnaire and mean results on QoL visual analogue scale (VAS) in children with no ventilation tube insertion (VTI) vs. VTI.
|
|
-VTI (n=346) |
+VTI (n=301) |
|
||
|
|
Mean (SD) |
CI |
Mean (SD) |
CI |
p-value |
|
Physical suffering |
1.23 (0.79) |
1.15-1.31 |
1.35 (0.81) |
1.26-1.45 |
0.052 |
|
Hearing loss |
1.28 (0.79) |
1.21-1-38 |
1.52(1.03) |
1.40-1.64 |
0.003 |
|
Speech impairment |
1.28 (0.85) |
1.19-1.37 |
1.51 (1.11) |
1.38-1.63 |
0.004 |
|
Emotional distress |
1.87 (1.20) |
1.75-2.00 |
2.21 (1.43) |
2.05-2.38 |
0.001 |
|
VAS |
0.94 (1.95) |
0.73-1.15 |
2.10 (2.83) |
1.77-2.43 |
<0.001 |
Table 5: Shows association of co-variables on child and family QoL.
|
|
QoL child |
QoL family |
||||
|
|
OR |
95% CI |
p-value |
OR |
95% CI |
p-value |
|
Allergy |
1.02 |
0.82-1.25 |
0.842 |
1.04 |
0.84-1.28 |
0.742 |
|
Asthma/ asthmatic bronchitis |
0.91 |
0.77-1.06 |
0.252 |
1.03 |
0.83-1.26 |
0.500 |
|
Atopic eczema |
1.08 |
0.94-1.24 |
0.277 |
0.95 |
0.79-1.10 |
0.541 |
|
Living with siblings |
0.97 |
0.79-1.20 |
0.831 |
1.05 |
0.90-1.21 |
0.710 |
DISCUSSION
We have in this study investigated how OM in children and VTI affects QoL in children and in their families in a rural population in Denmark by use of questionnaires and numerical VAS scales. LOFUS was initiated to create more knowledge on health aspects in a population living in a rural and socioeconomic more disadvantaged area compared to the previously collected Danish general population studies carried out in urbanized and richer areas of Denmark. OM is a frequent disease in especially children and known to affect the social life of the families with a child suffering from especially recurrent middle ear problems [11–15].
Our study adds to this knowledge. We found a high frequency (57%) of reported OM and more than one of five children have had >3 OM episodes. This is comparable to Danish nationwide data [1]. It has been reported that VTI treatment has positive effects on QoL in families [8,9]. Our study confirms that children living in a rural area who have been treated with VTI as well as their families have had significantly worse affected QoL compared to children without need for VTI. Also, our study confirms that the frequency of VTI is high (26% of children) and thus comparable to the rest of Denmark [1].
Previous studies have shown association between lower socioeconomic status and high BMI in children [26,27]. Also, other studies have shown association between childhood obesity and OM [23]. However, BMI was not in this study correlated to OM although overweight was. We have no explanations for this finding.
Incidence of OM decreases with increasing age in children [1]. Therefore, parental recall bias in older children on how many times their child has had OM, and how it affected QoL earlier in life is a limitation. Also, presence of siblings may introduce recall bias. Best practice for answering these questions would be a short period of time after ended OM episode. However, recently it has been shown that reportation of VTI is a reliable measure [1]. Another limitation is that due to the structure of the LOFUS cohort covering several other health areas in a comprehensive questionnaire, we were only allowed to include four of the original six questions from the OM-6 questionnaire. We chose to incorporate the items best describing QoL but still this limits comparison with other studies using OM-6.
The nature of the LOFUS questionnaires did not allow to differentiate between the types of OM. We assume the vast majority of VTI were bilaterally inserted but we do not have exact information on this. Number of individual VTI procedures or type of ventilation tubes used were not obtained.
Approximately 5% of persons invited to LOFUS were nonDanish citizens with varying Danish language proficiency [17]. However, it was decided that LOFUS could not prioritize resources for translation into relevant languages. Thus, only participants who mastered Danish could fill in the questionnaires [17], leading to selection bias concerning the population representation in the study. As in other population studies, it is expected that nonparticipants will have lower socioeconomic status, more illnesses and lower mean survival than participants [24].
We found rather large confidence intervals, and this indicates lack of power in our study with 1,169 participating children. LOFUS was a multipurpose cohort with invitations restricted to the Lolland-Falster population and therefore it was not possible to enroll a larger population. However, in total 33% of the population aged 0-14 years living in Lolland-Falster attended the LOFUS cohort.
CONCLUSION
Our study confirms a high frequency of reported OM and a high frequency of VTI procedures also in a rural population of Denmark. Furthermore, the study shows a significant correlation between VTI and poorer QoL in children and their families. Also, children with VTI compared to children without VTI score worse in three of four of the included modified OM-6 questions and on a QoL VAS-scale.
ACKNOWLEDGMENT
Lolland-Falster Health Study (LOFUS) is a collaboration between Region Zealand, Nykøbing Falster Hospital and Lolland and Guldborgsund municipalities. The authors are grateful for permission to use LOFUS data. Also, thanks to all the families who took time to answer the questions on otitis media in the LOFUS study. The analysis and interpretation of LOFUS data presented in this paper are the sole responsibility of the authors.
REFERENCE
- Todberg T, Koch A, Andersson M, Olsen SF, Lous J, Homøe P. Incidence of otitis media in a contemporary Danish National Birth Cohort. PLoS One. 2014; 9: 1–13.
- Pedersen TM, Mora-Jensen ARC, Waage J, Bisgaard H, Stokholm J. Incidence and determinants of ventilation tubes in Denmark. PLoS One. 2016; 11: 1–12.
- Ahmed S, Shapiro NL, Bhattacharyya N. Incremental health care utilization and costs for acute otitis media in children. Laryngoscope. 2014; 124: 301–5.
- Speets AM, Wolleswinkel JH, Forsgren A, Sobocki PA. Use of medical resources and indirect costs of otitis media in Sweden. Scand J Public Health. 2011; 39: 137–146.
- Lous J, Ryborg CT, Thomsen JL. A systematic review of the effect of tympanostomy tubes in children with recurrent acute otitis media. Int J Pediatr Otorhinolaryngol. 2011; 75: 1058–1061.
- Kørvel-Hanquist A, Koch A, Lous J, Olsen SF, Homøe P. Risk of childhood otitis media with focus on potentially modifiable factors: A Danish follow-up cohort study. Int J Pediatr Otorhinolaryngol [Internet]. 2018; 106: 1–9.
- Lanphear BP, Byrd RS, Auinger P, Hall CB. Increasing prevalence of recurrent otitis media among children in the United States. Pediatrics. 1997; 99: 1–7.
- Chow Y, Wabnitz DAM, Ling J. Quality of life outcomes after ventilating tube insertion for otitis media in an Australian population. Int J Pediatr Otorhinolaryngol. 2007; 71: 1543–7.
- Siggaard LD, Barrett TQ, Lüscher M, Tingsgaard PK, Homøe P. Parent satisfaction and symptom relief in children with otitis media undergoing tympanostomy tube insertion. Dan Med J. 2019; 66: 1–6.
- Hellström S, Groth A, Jörgensen F, Pettersson A, Ryding M, Uhlén I, et al. Ventilation tube treatment: A systematic review of the literature. Otolaryngol - Head Neck Surg. 2011; 145: 383–18.95.
- Heidemann CH, Lauridsen HH, Kjeldsen AD, Faber CE, Johansen ECJ, Godballe C. Caregiver quality of life and daily functioning in relation to ventilating tube treatment. Otolaryngol - Head Neck Surg (United States). 2014; 151: 341–7.
- Ryborg CT, Søndergaard J, Lous J, Munck A, Larsen P V., Thomsen JL. Quality of life in children with otitis media-a cohort study. Fam Pract. 2014; 31: 30–7.
- Heidemann CH, Lauridsen HH, Kjeldsen AD, Faber CE, Johansen ECJ, Godballe C. Quality-of-Life Differences among Diagnostic Subgroups of Children Receiving Ventilating Tubes for Otitis Media. Otolaryngol- Head Neck Surg (United States). 2015; 153: 636–43.
-
Rosenfeld RM, Bhaya MH, Bower CM, Brookhouser PE, Casselbrant ML, Chan KH, et al. Impact of tympanostomy tubes on child quality of life. Arch Otolaryngol - Head Neck Surg. 2000; 126: 585–92.
- Homøe P, Heidemann CH, Damoiseaux RA, Lailach S, Lieu JEC, Phillips JS, et al. Panel 5: Impact of otitis media on quality of life and development. Int J Pediatr Otorhinolaryngol [Internet]. 2020; 130: 1–10.
- Jepsen R, Egholm CL, Brodersen J, Simonsen E, Grarup J, Cyron A, et al. Lolland-Falster Health Study: Study protocol for a household-based prospective cohort study. Scand J Public Health. 2020; 48: 382–390.
- Egholm CL, Packness A, Stokholm J, Rasmussen K, Ellervik C, Simonsen E, et al. Questionnaire development for the Lolland-Falster Health Study, Denmark: An iterative and incremental process. BMC Med Res Methodol. 2020; 20: 1–7.
- Heidemann CH, Godballe C, Kjeldsen AD, Johansen ECJ, Faber CE, Lauridsen HH. The Otitis Media-6 questionnaire: Psychometric properties with emphasis on factor structure and interpretability. Health Qual Life Outcomes. 2013; 11: 1–10.
- Ministry of the Interior and Housing. Key figures of municipalities[Public Database], 2020. 2020.
- Mei Z, Scanlon KS, Grummer-Strawn LM, Freedman DS, Yip R, Trowbridge FL. Increasing prevalence of overweight among US low-income preschool children: the Centers for Disease Control and Prevention pediatric nutrition surveillance, 1983 to 1995. Pediatrics. 1998; 101: 1–6.
- Wake M, Hardy P, Canterford L, Sawyer M, Carlin JB. Overweight, obesity and girth of Australian preschoolers: Prevalence and socio- economic correlates. Int J Obes. 2007; 31: 1044–51.
- Statistics NC for H. Vital and Health Statistics, Series 11, No. 246 (5/2002)--updated 6/30/2010 [Internet]. Vol. 11, Vital and Health Statistics, Series 11, No. 246 (5/2002)--updated 6/30/2010. 2002;1-189.
- Sidell D, Shapiro NL, Bhattacharyya N. Obesity and the risk of chronic rhinosinusitis, allergic rhinitis, and acute otitis media in school-age children. Laryngoscope. 2013; 123: 2360–3.
- Langhammer A, Krokstad S, Romundstad P, Heggland J, Holmen J. The HUNT study: Participation is associated with survival and depends on socioeconomic status, diseases and symptoms. BMC Med Res Methodol. 2012; 12: 1–14.