Pediatric Post Intubation Obstructive Fibrinous Tracheal Pseudomembrane
- 1. Department of Otolaryngology Head and Neck Surgery, University of Illinois at Chicago, USA
- 2. Department of Otolaryngology Head and Neck Surgery, Mount Sinai Hospital, USA
- 3. Department of Pediatric Otolaryngology, Anne & Robert H. Lurie Children’s Hospital of Chicago, Northwestern University, USA
CITATION
White Z, Sapthavee A, Jajoo D, Schroeder JW Jr. (2016) Pediatric Post Intubation Obstructive Fibrinous Tracheal Pseudomembrane. Ann Otolaryngol Rhinol 3(6): 1115.
INTRODUCTION
Endotracheal intubation is a safe and commonly used procedure to maintain the airway during general anesthesia, to protect the airway during surgery, and as a means to provide respiratory support for patients in respiratory failure, however it is not without complications. Laryngeal and tracheal stenosis, tracheal ulcers, laryngeal granuloma and acquired tracheomalacia are all well recognized complications of intubation [1, 2]. One less frequent and often unrecognized but potentially fatal complication of endotracheal intubation is obstructive fibrinous tracheal pseudomembrane (OFTP) formation. It is rare especially in the pediatric population. We present a case of OFTP in a pediatric patient and a review and analysis of all previous cases (adult and pediatric) of OFTP reported in the literature.
CASE PRESENTATION
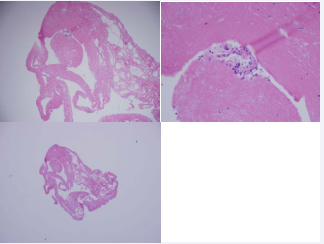
A 14 year old previously healthy female, who was in a pedestrian versus automotive trauma was found unresponsive at the scene of accident with agonal breathing. King airway (a supraglottic airway) was used to ventilate her during transport to the emergency department (ED) of an outside hospital. She was intubated in the ED with a 7.5mm endotracheal tube without difficulty. A detailed trauma workup was done, and other than fracture of right thumb, no major injury was found. On hospital day 2, about 23 hrs, after intubation, she was extubated. She developed a persistent cough within hours after extubation, which progressively worsened over next 3 days. Intermittent biphasic stridor was noted on 2nd day after extubation, and by the 3rd day her stridor became persistent. She was treated with intravenous dexamethasone 5mg every 8 hours (3 doses), vancomycin, piperacillin/tazobactam and nebulized racemic epinephrine without any improvement. On the 3rd day the otolaryngology service was consulted. Stridor and suprasternal retractions were noted on examination. Flexible fiber optic laryngoscopy was done at the bedside. The Nasopharynx, oropharynx, supraglottis, and glottis were normal in appearance with normal vocal cord mobility. However, there was what appeared to be a whitish membrane, partially visualized in the subglottis. The decision was made to take the patient to the operating room for diagnostic bronchoscopy. A Miller 3 blade was used to perform direct laryngoscopy, and upon visualization the subglottic airway was noted to be narrowed. A 5mm rigid endoscope was passed through the vocal cords and into the subglottis. A thick, circumferential, whitish membrane was visualized in the subglottis and it extended inferiorly into the mid trachea. The pseudomembrane material was firm and dense and not able to be removed with a suction catheter. A cup forceps was used to biopsy a small amount of the exudate and it was sent for analysis [3,4]. Pathologic analysis demonstrated fibrin with focal acute inflammation, consistent with fibrinous pseudomembrane (Figure 1).
Figure 1: Histopathological slides consistent with inflammatory fibrinous tissue.
The patient was reintubated with a 5.0 mm endotracheal tube and the cuff was left deflated as there was no leak below 25 cm/H2 0. , The patient was transferred back to the intensive care unit sedated, intubated and ventilated. She was given intravenous vancomycin and cefepime and intravenous dexamethasone was given in doses of 4 mg 6 hourly. Two days after reintubation, patient’s respiratory status deteriorated. A chest x-ray demonstrated complete atelectasis of right lung. She then developed cardiac arrest, requiring cardiopulmonary resuscitation. During resuscitation, pneumothorax was suspected, and bilateral chest tubes were placed. Repeat chest x-ray showed pneumomediastinum, subcutaneous emphysema and expansion of right lung. Once patient was stabilized, she was transferred to a tertiary care children’s hospital for further work up and intervention.
On presentation at the pediatric hospital, a CT scan of the larynx was performed due to concern for possible laryngeal fracture sustained at the original trauma which may have caused the subglottic narrowing. The scan did not demonstrate a fracture. The patient’s respiratory status improved (was on minimal ventilatory support and the chest tubes had been removed) and on hospital day two, the patient was taken to the operating room for diagnostic bronchoscopy. A 4 mm Hopkins rod telescope was used to visualize the larynx which was exposed with a large lindholm laryngoscope. There were posterior glottic furrows and tongues of granulation tissue (Figure 2).
Figure 2: View on Laryngoscopy.
A bronchscopy performed with the 4mm Hopkins rod telescope demonstrated a circumferential, white, firm ring at the level of the cricoid (Figure 3),
Figure 3: Subglottic narrowing with white circumferential membrane.
this was not able to be removed with suction. At this time it was postulated that this patient likely had a congenitally small cricoid and that the initial intubations with larger tubes caused pressure necrosis leading to the white appearance of the subglottic. The patient was transferred back to the PICU extubated. There was no respiratory distress but she did have a hoarse voice. On hospital day 3 the patient had minimal stridor but no increased work of breathing and was saturating over 96% on room air. She underwent bedside flexible fiberoptic laryngoscopy that again demonstrated the subglottic narrowing. Patient continued to do well and underwent repeat bronchoscopy before she was transferred out of the intensive care unit to ensure her airway was healing. On this bronchoscopy, the white gelatinous ring was again appreciated and this time was able to be debrided with forceps [5,6]. The circumferential exudate was entirely debrided from the subglottis to the mid trachea. The exudate was sent to pathology as well as to microbiology for analysis. Healthy cricoid and tracheal mucosa without narrowing were exposed (Figure 4).
Figure 4:Tracheal wall after bronchoscopic removal of membrane.
Pathology on this specimen was consistent with fibrinopurulent exudate. The patient did well post-operatively and was without stridor, oxygen requirement or increased work of breathing, and was discharged home. The patient was brought back to the operating room six weeks later for follow-up laryngoscopy and bronchoscopy, A 4.0 telescope was used to obtain a magnified view of the larynx. The laryngeal, tracheal and bronchial mucosa was normal. There was no narrowing (Figure 5).
Figure 5: Tracheal wall on follow-up bronchoscopy 6 weeks after discharge.
METHODS
A PubMed search for obstructive fibrinous tracheal pseudomembrane and tracheal pseudomembrane was conducted. 19 individual case reports and 7 case series were found in the English literature. 2 other case reports, which were published in German, but was included in the analysis of 2011 literature review on this topic by Lins etal [4], were also included. All these articles were carefully studied to ensure that the pseudomembrane described was not caused by infection or some other known cause. The data was collected and compiled into table 1 (including our case) for analysis (total 55 cases). There were 2 other publications, that made mention of cases of OFTP, but did not have enough details of the case, to be included in our analysis [7,8] .
RESULTS
The patients described in the reports ranged from 6wk to 85yrs in age, with an average age of 34.34 yr (±25.6). 33 subjects were females and 22 were males. The reason for intubation varied, 5 patients intubated due to trauma related complications, 9 had conditions that lead to altered sensorium, 15 had conditions that resulted in respiratory failure, 21 had intubations done for surgical procedure, 2 had intubations done as part of cardiopulmonary resuscitation, 1 intubated due to heart failure and 1 for eclampsia (Table 1). The duration of intubation ranged from 30 minutes to 17 days, with average time of 76.24 hours (±103.72). The duration from extubation until onset of symptoms was almost immediate to 2 weeks, with average time of 52.30 hours (±73.51).
Most patients presented with stridor and respiratory distress that began in post-extubation period and in some of these cases, the stridor and dyspnea was reported to be intermittent and positional. In a few cases wheezing was reported (case 36, 37, 44). Severe cough was also reported as concerning symptom in some cases. In one case (case 4), authors described clinical picture of progressive respiratory failure [9,10]. In 3 cases (cases 7, 11, 41), OFTP was an incidental finding on bronchoscopy done for evaluation of atelectasis.
Analysis of these cases did not identify any clear-cut risk factors predisposing to the development of OFTP. In the majority of the reported cases the patients were intubated with cuffed endotracheal tube. However, there were 10 cases (case 15, 43, 54, 29-35) in which authors explicitly mentioned use of uncuffed endotracheal tube, and in 7 cases (case 18, 21-25, and 51) use of high volume, low pressure cuff was described. Laryngeal trauma was described in one case (case 2), traumatic or difficult intubation was noted in 5 cases (case 14,28,35,36,46), multiple intubations in 5 cases (case 16,19,27,36,41), use of large ET tube in one case [11,12], and repeated movement of ET tube in 2 patients (case 15 & 54). In one case ET tube was used in prone position for back surgery (case 40). In 2 cases (case 19 & 36), clinical picture was suggestive of aspiration. 5 cases (case 16, 17, 22, 26, 27) had clinical picture associated with circulatory hypoperfusion, and 6 patients (case 11, 21, 37, 38, 42, 51) had Diabetes.
After onset of post-extubation symptoms, 12 patients were reintubated and 2 had temporary tracheostomy done, prior to undertaking other diagnostic and therapeutic measures. In 21 cases, rigid bronchoscopy was used first for removal of membrane. In 19 cases, flexible bronchoscopy was used first, which was successful in complete ablation of membrane in 16 cases. In another 3 cases, flexible bronchoscopy was not able to remove the membrane (case 36, 37 and 40). In 5 cases, bronchoscopy is mentioned as the tool used for removal of membrane, without specifying if it was flexible or rigid bronchoscopy. In 4 cases, membrane was spontaneously expectorated with vigorous cough, with improvement in symptoms. In one case, only medical treatment was used (case 41), with resolution of membrane when seen in repeat bronchoscopy [13,14]. In one case (case 44), after finding a mucosal flap in distal trachea on rigid bronchoscopy, flexible bronchoscopy was used to guide placement of endotracheal tube distal to the obstructing membrane. After few days, repeat bronchoscopic examination after withdrawal of endotracheal tube showed that mucosal flap had aligned and adhered to the tracheal wall with marked improvement in tracheal lumen. Patient was then kept extubated, and made full recovery. In one case (case 51), patient was intubated, but had difficult ventilation through the endotracheal tube, so the endotracheal tube was immediately removed. It was then found, that there was a tubular membrane at the tip of tube completely blocking it. In one case (case 49) tracheostomy was done, and then membrane was removed through the tracheostomy tube. In 2 cases (case 2 & 13), no intervention could be attempted prior to death, and diagnosis was made on autopsy [15,16].
In those cases, where intervention was achieved with the use of bronchoscopy, in majority, forceps were used for removal of membrane, but in some cases other techniques were used. With the use of flexible bronchoscopy, removal in some cases was achieved with the use of scraping with brush (case 16), cryotherapy (case 26), balloon (case 31, 32 & 35) and laser (case 29, 33 & 34). With the use of rigid bronchoscopy, removal in one case was done with the use of cold instruments (case 20), and in another case with the use of snare, electro cautery and argon plasma coagulation (case 27).
In 17 cases (including the case report described above), a repeat bronchoscopy was done 3 days – 4months after resolution of symptoms. In one case (case 20), asymptomatic grade 1 subglottic stenosis was noted, but in all others, no abnormality was seen [17-19].
In most cases, OFTP was described to be present in subglottis and/or proximal trachea, but in 3 cases it was noted in mid trachea (case 38, 41, 42), in 2 cases in distal trachea (case 21 & 44) and in one case it was described to be present at carina and deeper in the major airways (case 23). The color of the lesion is reported to be whitish in most cases, but in few cases, it was described to be of gray (case 14 & 52), yellow (case 30, 31 & 38) or pink color (case 29 & 32). Four major types of morphology have been described: 1. circumferential tubular membrane coating the inner wall of trachea with only one central lumen. 2. Valve like septal membrane attached to a part of trachea and floating into its lumen, and transversely dividing tracheal lumen [20,21]. 3. Mixed-type, with circumferential membrane, which is partially detached from its proximal part and is floating. 4. Bridge like transverse membrane connecting opposite walls of trachea. This has been reported only in 2 patients (case 20 & 41).
Histopathology of lesion was described in 41 cases. All were reported to have fibrinous material and most others also had inflammatory cells and/or epithelial cells.
Overall, 49 patients (89%) made full recovery, 3 patients died, 1 patient left against medical advice and was lost to follow-up, one needed long-term tracheostomy due to persistent coma, and one infant developed asymptomatic grade 1 subglottic stenosis.
DISCUSSION
Obstructive fibrinous tracheal pseudomembrane is a rare but potentially serious complication of endotracheal intubation. A typical case of OFTP presents with stridor and respiratory distress shortly after extubation, a presentation shared by many other common and well known etiologies such as airway edema, laryngospasm, bronchospasm, vocal cord dysfunction, ulcers, granuloma, tracheomalacia or retention of secretions [22-26]. In some cases clinical picture may be inconsistent or misleading, when valve like obstruction may result in positional and intermittent dyspnea or when patient is too exhausted to generate stridor [27-29]. Lack of distinguishing clinical features between OFTP and other common etiologies result in inaccurate initial diagnosis, as was the situation in the case presented above leading to delayed diagnosis and treatment. It is therefore important that bronchoscopy be considered in all cases of post extubation respiratory distress, if they are not responding to medical treatment of common etiologies.
Although OFTP is infrequently described, it is likely under recognized. In many cases, symptoms of OFTP are attributed to other well-known etiologies. In many of the cases reviewed, treatment for possibility of laryngeal edema and/ or bronchospasm was given with use of nebulized epinephrine, nebulized albuterol and systemic steroids without improvement in clinical picture, before the true problem was addressed. If patients fail medical therapy many are reintubated, which may dislodge or remove the membrane, and thus condition may remain unrecognized [2,4]. It is also possible (as described in case 44), that in some cases reintubation results in displacement of valve like membrane in a manner, that it aligns and adheres to tracheal wall with improvement in obstruction. Many cases of OFTP may be silent, as the membrane may not be of enough thickness to cause obstruction, or may not detach to cause valve like obstruction. This is supported by those 3 cases, in which OFTP was found as an incidental finding on bronchoscopy done for other reason. 4 cases in this review, has been reported to resolve with spontaneous expectoration of membrane. It is possible, that there are many other cases, where such expectoration of membrane with coughing was not recognized.
The pathophysiology of this condition is not clear. It is thought to occur secondary to tissue ischemia from compression of tracheal mucosa by the endotracheal tube itself or its cuff, typically resulting in circumferential injury to mucosa of subglottic area and adjoining proximal trachea. The majority of patients presented were intubated with a cuffed endotracheal tube which raised the concern that increased cuff pressure might have initiated the tracheal injury leading to OFTP formation. In areas of mucosal injury, leaked and deposited fibrinous tissue combined with necrotic epithelium and inflammatory cells forms a membrane-like structure that initially coats the surface of the mucosa. After extubation, either by mechanical pull of endotracheal tube or by subsequent coughing manipulation, in some cases, membrane may detach from its proximal part and float downwardly inside the lumen to form a ball-valve like membrane [5].
Histopathology of the lesion typically shows fibrinous material admixed with inflammatory cells and necrotic epithelial cells. They do not contain sub-epithelial stromal tissues. This suggest that OFTP, is the result of superficial injury to tracheal mucosa [4]. This is also supported by the finding, that removal of OFTP is associated with very high rates of full recovery without any residual obstruction. Pressure on deeper tissues results in more intense inflammatory response, healing with fibrous scar formation, and resulting in tracheal stenosis [5].
No clear pattern of risk factor that might increase chance of development of OFTP emerged from analysis of 55 cases included in this review. OFTP occurred in all ages (6weeks – 84 year), in cases with both brief and long duration of intubation (duration range of 30 minutes to 17 days), and with various types of indications for intubation. This suggests that age, duration of intubation or underlying conditions that necessitated intubation, do not appear to be significant risk factors. Increased endotracheal tube cuff pressure can increase the risk of mucosal injury, but in our review, despite use of uncuffed tube in 10 cases, and use of high volume, low pressure cuff in 7 cases, OFTP still developed. Other risk factors for mucosal injury such as difficult or traumatic intubation, repeated intubations, excessive manipulation of tube, use of large size endotracheal tube, and aspiration of gastric contents were noted in some cases, but many others did not have these issues. Therefore, it remains unclear, why OFTP occurs in few patients, and not in large number of others, who are intubated.
Although some cases improved with spontaneous expectoration of membrane, most needed intervention with bronchoscopy for its removal. Both rigid and flexible bronchoscopy has been used to remove the membrane. Rigid bronchoscopy was successful in membrane ablation in all cases. Flexible bronchoscopy was also associated with high success rate, but in 3 cases needed complement of rigid bronchoscopy. Some authors [2,4] feel that removal of lesion with rigid bronchoscope is easier and faster than the use of flexible bronchoscope, and provides better control of ventilation during the procedure. But others [5] feel quite skilled in removing them by flexible bronchoscope with use of non-invasive ventilation during the procedure, and were able to achieve complete ablation in 15- 25 minutes. Therefore, choice of procedure would depend on expertise and preference of local expert.
CONCLUSION
OFTP is an infrequently described, likely under recognized, potentially life-threatening complication of endotracheal intubation. It is clear from our case presentation that correct diagnosis and treatment of the condition was delayed due to the under recognized nature of the condition and therefore it is important to discuss in the literature. No clear risk factor that increase chances of OFTP is known and therefore the condition needs to be considered in all cases of post-extubation respiratory distress, occurring immediately or up to few weeks after extubation, in which no other cause for symptoms are apparent. Bronchoscopy helps in diagnosis and removal of lesion and is associated with high rates of full recovery without sequelae.
REFERENCES
13. Berger TM, Jöhr M. Subglottic fibrinous cast. Paediatr Anaesth. 2005; 15: 622-623.
17. Birch CW, Salkeld LJ. A rare tracheal lesion. Paediatr Anaesth. 2005; 15: 73-76.
18.Gershman A, Githaiga A, Mehta A. Pseudomembranous tracheal stenosis. J Bronchol. 2006; 13: 82–83.
21. Carron K, Violon D. Post intubation tracheal pseudomembrane. J Bronchol. 2007; 14: 210–211.
ABSTRACT
Objectives: Report a rare case of obstructive fibrinous tracheal pseudomembrane (OFTP) in a pediatric patient and to present a literature review on OFTP.
Methods: A PubMed search was conducted which revealed a total of 21 individual case reports and 6 case series of OFTP. Relevant data was collected from these publications and analyzed.
Results: 55 patients with OFTP were identified. Age ranged from 6wk to 85yr, with mean age (± SD) of 34.34 yr (±25.6). 33 were female and 22 were male. The reason for initial intubation varied, and included trauma (n=5), altered sensorium (n=9), respiratory failure (n=15), and intubation for surgical procedure (n=21). The duration of intubation ranged from 30 minutes to 17 days, with mean duration (±SD) of 76.24 hours (±103.72). The duration from extubation until onset of symptoms was almost immediate to 2 weeks, with mean duration (±SD) of 52.30 hours (±73.51). No clear risk factor for development of OFTP was identified. Majority of patients, 45/55 (82%), were treated with bronchoscopy. Most patients, 49/55 (89%), recovered, without any sequelae, but there were few deaths, 3/55 (5%).
Conclusion: OFTP is a rare, but serious and potentially life threatening cause of post extubation respiratory distress. No risk factor could be identified which may predispose to development of OFTP. Bronchoscopy confirms the diagnosis and removal of the fibrinous exudate is associated with a high rate of recovery without sequelae.
KEYWORDS
• Tracheal pseudomembrane
• Post-intubation obstruction
• Fibrinous tracheal Pseudomembrane
• Obstructive fibrinous tracheal pseudomembrane