Temporomandibular Joint Subluxation: A Less Invasive Approach for Accessing the Parapharyngeal Space and Limited Middle Skull Base Compared to Mandibular Osteotomies
- 1. Oral and Maxillofacial Surgery Unit, Christian Medical College and Hospital Vellore, India
INTRODUCTION
The parapharyngeal space and middle skull base harbour critical neurovascular structures and are challenging to access surgically. Traditional approaches, such as mandibular osteotomies (swing, segmental, or sagittal split), have been the mainstay for extensive access. However, these techniques require significant manipulation of the mandible and associated structures, leading to increased surgical trauma, risk of infection, and longer recovery times [3]. TMJ subluxation, achieved through controlled intraoperative displacement of the mandibular condyle, offers an alternative approach that reduces surgical invasiveness while maintaining adequate exposure for select cases [4].
TMJ Subluxation as a Surgical Approach
TMJ subluxation involves anterior translation of the mandibular condyle beyond the articular eminence, temporarily elongating the mandible without permanent dislocation. This manoeuvre increases intraoral and transoral visibility of the PPS and limited portions of the MSB without requiring osteotomies or extensive soft tissue dissection [5].
Technique
Direct wiring is done in relation to the lower canine, premolar region on the side of the preferred dislocation and one direct wiring is done in relation to the opposite side upper canine and premolar region. These direct wirings are twisted together, as done for intermaxillary fixation with mouth in a closed position. This will cause the movement of the lower canine to the midline, which causes the subluxation of the joint. This will provide an access of approximately 1cm. In case of absence of teeth, Temporary Anchorage Devices (TADs) can be used. Once the surgery is completed, the inter maxillary fixation can be released and joint falls back into the socket.
Advantages
1. Minimally Invasive – Unlike mandibular osteotomies, TMJ subluxation does not require bone cutting or fixation, reducing operative time and recovery duration.
2. Reduced Morbidity – Avoids complications such as non-union, malocclusion, and nerve injury commonly associated with osteotomies [6].
3. Enhanced Surgical Access – Provides direct visualization and instrument manoeuvrability for parapharyngeal lesions with limited involvement of the MSB.
4. Preservation of Jaw Function – Since no osteotomy is performed, patients experience less postoperative discomfort and earlier return to function.
4. Limitations and Considerations
• Limited Exposure to the MSB – While effective for the PPS, TMJ subluxation provides restricted access to deeper skull base structures compared to osteotomies.
• Patient Selection – Not all patients are candidates; TMJ hypermobility, pre-existing joint disorders, and extensive tumor involvement may preclude this approach.
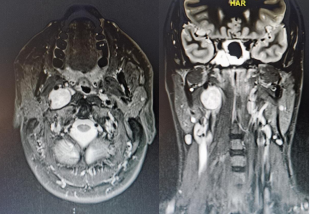
Figure 1: The location of the lesions in the infratemporal region that can be accessed with TMJ subluxation, without mandibular access osteotomy.
Figure 2: The method of TMJ subluxation; A. Placement of direct wiring in relation to mandibular canine premolar region of the side of TMJ subluxation and on the opposite side in the maxillary arch. B. Direct wiring placed are intertwined with each other to create TMJ subluxation. Note the position of the lower teeth in relation to maxillary teeth after the subluxatio
CONCLUSION
TMJ subluxation presents a valuable, less invasive alternative for accessing the PPS and selected portions of the MSB compared to traditional mandibular osteotomies. While it offers reduced morbidity and preserves jaw function, its application remains case-dependent and may not completely replace osteotomies for extensive skull base exposure. Further studies and clinical experience will refine patient selection criteria and optimize its utility in maxillofacial and skull base surgery.