Tuberculous Otitis Media Involving the Temporomandibular Joint: A Case Report
- #. Yuting Tao and Yuqi Men have contributed equally to this work and share first authorship.
- 1. Department of Otolaryngology-Head and Neck Surgery, Peking University People’s Hospital, China
- 2. Department of Clinical Science, Intervention and Technology, Karolinska Institute, Sweden
- 3. Department of Otolaryngology Head and Neck Surgery & Audiology and Neurotology, Karolinska University Hospital, Sweden
Abstract
Tuberculous otitis media (TBOM) is a rare form of extrapulmonary tuberculosis. The secondary involvement of the temporomandibular joint (TMJ) from TBOM has hardly been reported. This article presents the clinical features, diagnosis and therapy of a rare case of tuberculous otitis media with TMJ involvement. The diagnosis of TBOM with TMJ involvement was definitely established by a positive Mycobacterium tuberculosis nucleic acid amplification test on the surgical biopsy specimen. The patient reported relief of otalgia and otorrhea following the surgery combined with anti-tuberculosis drugs. We highlight the importance of nucleic acid amplification in the diagnosis of TBOM when traditional staining and culture methods return negative results. Although TMJ tuberculosis secondary to TBOM is extremely rare, a combination of anti-tuberculosis therapy and timely surgical intervention is necessary for refractory cases.
Keywords
• Extrapulmonary tuberculosis; Temporomandibular joint; Otitis medi; Temporomandibular joint arthritis; Tuberculosis
Citation
Tao Y, Men Y, Han L, Diao T, Yu L, et al. (2025) Tuberculous Otitis Media Involving the Temporomandibular Joint: A Case Report. Ann Otolaryngol Rhinol 12(5): 1369.
INTRODUCTION
Tuberculous otitis media (TBOM) is an uncommon form of extrapulmonary tuberculosis, which often presents as painless otorrhea, multiple tympanic membrane perforations and severe hearing loss at an early stage [1]. But the clinical manifestations have become variable nowadays due to the widespread use of antibiotics, making early diagnosis increasingly challenging. Additionally, TBOM might spread and impair other parts of head and neck region. However, temporomandibular joint (TMJ) tuberculosis secondary to TBOM has not been reported.
In this article, we reported an extremely rare case of TMJ tuberculosis secondary to tuberculous otitis media and described the diagnosis and treatment in detail.
CASE PRESENTATION
A 65-year-old female presented to our hospital for right ear discharge and otalgia. She experienced intermittent otorrhea for 20 years and reported right sided tinnitus, hearing loss, and otalgia with no response to antibiotics. She felt pain while opening her mouth. She had lost 5 kilograms in the past four months. The medical history included diabetes, coronary atherosclerotic heart disease with cardiovascular stent implantation, total hip arthroplasty on the right side, and hypertension.
White, thin secretions were observed in the swollen right external auditory canal (EAC), along with a large perforation of the tympanic membrane and granulation in the tympanic cavity. Right-sided TMJ tenderness was noted without facial swelling.
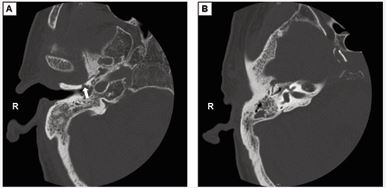
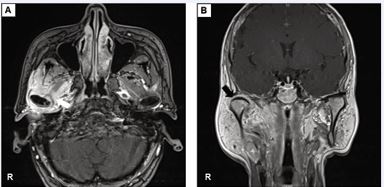
An erythrocyte sedimentation rate of 54 mm/h was detected, with normal results for the complete blood count and C-reactive protein. A computed tomography (CT) scan showed low-density shadows in the right tympanic cavity and mastoid process, bony erosion in the anteroinferior wall of EAC leading into the mandibular fossa, and massive low-density shadows around the condyle [Figure 1]. Magnetic resonance imaging (MRI) with contrast exhibited enhancement around the right TMJ and adjacent muscles [Figure 2].
Figure 1 The computed tomography scan of the patient. (A) The bone destruction formed a sinus (the arrow) from the anteroinferior wall of EAC to the mandibular fossa. (B) Inflammatory tissue filled the tympanic sinus, tympanum and mastoid process.
Figure 2 Magnetic resonance imaging (MRI) with contrast of the maxillofacial region. (A) The axial view showed peripheral enhancement signals of the right temporomandibular joint and surrounding muscles (white arrow). (B) The coronal view exhibited swollen inflammatory tissue around the mandibular condyle (black arrow).
The ear smear showed a sterile specimen. The posteroinferior swollen skin of the right EAC and granulations of the tympanic cavity were excised for biopsy, the acid-fast bacilli staining returned a negative result. However, the T-SPOT. TB test was positive. The patient was discharged for anti-tuberculosis treatment in specialized hospital yet didn’t take anti-tuberculosis medications. Her otalgia, occlusal pain, and otorrhea exacerbated with a newly presented right-sided headache one month later.
The right mastoidectomy was performed. Numerous granulations in the mastoid, epitympanum and tympanic antrum were cleared for pathology and microbiological culture. The TMJ exploration was conducted by a preauricular approach. Bony necrosis in the anterosuperior wall of the tympanum and the condyle of the TMJ was removed. Granulations on the surface of the temporomandibular joint capsule were sent for microbiological examination, quantitative real-time polymerase chain reaction (qPCR) for TB DNA detection. The qPCR of biopsy specimen reported a positive result which confirms the diagnosis of TBOM involving the TMJ. The patient went to the specialized hospital for treatment and the follow-up after 1 year showed the middle ear cavity epithelialized without drainage.
DISCUSSION
TBOM is an infrequent extrapulmonary involvement of tuberculosis found mostly in developing countries, accounting for 0.1% of all TB patients [2]. A review study on the reported cases of tuberculous otitis media summarized approximately 267 cases [3]. While primary TMJ tuberculosis is also rare, with approximately 20 reports reported since 1951 [4], the secondary involvement of the TMJ from TBOM is a clinical rarity.
Septic arthritis of the TMJ is known as a rare complication of otitis media. Potential routes of direct dissemination include opened squamotympanic fissures, incomplete ossification of tympanic plate, Santorini’s fissures (natural openings in the lateral cartilaginous auditory canal), Huschke’s foramens [5,6]. Tuberculosis of the temporomandibular joint and parotid secondary to TBOM was reported by merely one study [7]. In that case, a sinus from the anterior wall of external auditory canal to the TMJ was observed. Similarly, in our study, the infection perhaps spread to TMJ via a sinus from the anteroinferior wall of EAC which was observed in the CT scan.
The diagnosis of TBOM is often challenging. While the tuberculin skin testing and the interferon gamma release assays (IGRAs, including T. SPOT.TB and QuantiFERON assays) are commonly applied in the detection of latent TB, false positive results can be found in vaccinated people or patients who once had tuberculosis, and activity of the disease cannot be identified [8]. The definite diagnosis traditionally relies on the culture of Mycobacterium tuberculosis. However, this method requires more than 2 weeks and the positive rate is relatively low [9]. The acid fast bacilli staining is convenient but has an even lower sensitivity [2]. In this context, nucleic acid amplification techniques like qPCR are of great help, providing rapid results from small sample volumes with high sensitivity and specificity. In this case, despite negative findings from two pathological biopsies and acid-fast bacilli staining, the positive qPCR result of TB DNA detection confirmed the diagnosis.
The cornerstone of treatment for any form of tuberculosis is long-term, multi-drug anti-tuberculosis therapy. Surgical intervention plays a crucial role in managing complicated cases by debriding necrotic tissue, draining abscesses, and definitive diagnosis. Thus, we recommend surgical excision combined with anti-tuberculosis medications as a proper treatment for refractory cases such as in this report [10].
CONCLUSION
Mycobacterium tuberculosis infection should beconsidered when patients with chronic suppurative otitis media demonstrate no response to empirical medications. When TBOM is highly suspected, qPCR might be of great value. TMJ tuberculosis secondary to TBOM is extremely rare. Anti-tuberculosis therapy should be initially applied, and surgery is suitable for recurrent TMJ involvement.
ETHICS STATEMENT
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional guidelines on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008. This research was approved by the Administration Committee of Peking University People’s Hospital, China (2021PHB149). The written informed consent was obtained from the patient for her medical data to be published.
FUNDING
This work was supported by Peking University People’s Hospital Scientific Research Development Funds (RDY2021–25, RDZH 2022-01, RDE2022-37).
REFERENCES
- Suárez I, Fünger SM, Kröger S, Rademacher J, Fätkenheuer G, RybnikerJ. The Diagnosis and Treatment of Tuberculosis. Dtsch Arztebl Int. 2019; 116: 729-735.
- Velepic M, Vukelic J, Dvojkovic Z, Skrobonja I, Braut T. Middle east tuberculosis in an immunocompromised patient: Case report and review of the literature. J Infect Public Health. 2021; 14: 139-142.
- Pai KK, Omiunu AO, Peddu DK, Au VH, Baredes S, Jyung RW, et al. Tuberculosis of the middle ear: A systematic review. Am J Otolaryngol. 2022; 43: 103571.
- Assouan C, Anzouan K, Nguessan ND, Millogo M, Horo K, Konan E, et al. Tuberculosis of the temporomandibular joint. Rev Stomatol Chir Maxillofac Chir Orale. 2014; 115: 88-93.
- Dingle AF. Fistula between the external auditory canal and the temporomandibular joint: a rare complication of otitis externa. J Laryngol Otol. 1992; 106: 994-995.
- Kumar R, Hota A, Sikka K, Thakar A. Temporomandibular joint ankylosis consequent to ear suppuration. Indian J Otolaryngol Head Neck Surg. 2013; 65: 627-630.
- Prasad KC, Sreedharan S, Prasad SC, Chakravarthy Y. Tuberculosis of the temporomandibular joint and parotid secondary to tuberculous otitis media. Otolaryngol Head Neck Surg. 2007; 137: 974-975.
- Fu Y, Gong S. Tuberculosis otitis media. Chinese J Otorhinolaryngol Head Neck Surgery. 2007; 42: 471-473
- Hongler J, Musaazi J, Ledergerber B, Eberhard N, Sekaggya-Wiltshire C, Keller PM, et al. Comparison of Löwenstein-Jensen and BACTEC MGIT 960 culture for Mycobacterium tuberculosis in people living with HIV. HIV Med. 2018; 19: 654-661.
- Helbling CA, Lieger O, Smolka W, Iizuka T, Kuttenberger J. Primary tuberculosis of the TMJ: presentation of a case and literature review. Int J Oral Maxillofac Surg. 2010; 39: 834-838.es