2022 Volume 9 - Issue 2
-
October 31, 2022 Research Article
 Abstract Animal studies have shown that dietary probiotics can modify host stress response viathe gut-brain axis. A few studies with healthy human subjects have indicated that single strain fermented milk probiotic products can alter stress response. The aim .....
Abstract Animal studies have shown that dietary probiotics can modify host stress response viathe gut-brain axis. A few studies with healthy human subjects have indicated that single strain fermented milk probiotic products can alter stress response. The aim ..... -
November 30, 2022 Review Article
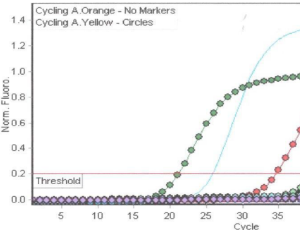 Abstract This study describes the development of a cost-effective, multiplex Loop-Mediated Isothermal Amplification (LAMP) method for detection of toxigenic Clostridioides difficile from diarrheal stools and presumptive identification of the NAP-1 strain. The.....
Abstract This study describes the development of a cost-effective, multiplex Loop-Mediated Isothermal Amplification (LAMP) method for detection of toxigenic Clostridioides difficile from diarrheal stools and presumptive identification of the NAP-1 strain. The..... -
December 16, 2022 Review Article
 Abstract GI tumors until now remain the major health problem in the world. The numerous risk factors are related to the development of GI tumors. Vitamin D is a multifunctional hormone with functions including immunomodulation or antioxidants to several intra.....
Abstract GI tumors until now remain the major health problem in the world. The numerous risk factors are related to the development of GI tumors. Vitamin D is a multifunctional hormone with functions including immunomodulation or antioxidants to several intra..... -
December 16, 2022 Short Communication
 Abstract Objective: Assess if the addition of rituximab to a dose-dense chemotherapy regimen in patients with primary gastric diffuse large B-cell lymphoma (PGL) in early stage, but associated with worse prognostic factors. Patients and methods: Patients wit.....
Abstract Objective: Assess if the addition of rituximab to a dose-dense chemotherapy regimen in patients with primary gastric diffuse large B-cell lymphoma (PGL) in early stage, but associated with worse prognostic factors. Patients and methods: Patients wit.....