Investigating Factors Associated With Pneumonectomy and Assessing Short-Term Outcomes: A Five-Year Retrospective Case- Control Study
- 1. Mekonnen Feyissa, Adama hospital Medical College, Adama, Ethiopia
ABSTRACT
Background: Pneumonectomy is the surgical removal of the entire lung, first performed in 1933 by Evarts A. Graham for lung carcinoma. It is associated with high morbidity and mortality compared to other minimal lung resections.
Objectives: The aim of this study is to investigate factors associated with pneumonectomy and its outcome assessment among patients for whom Lung resection done in TASH from January 2017 to December 2022.
Methods and Materials: A retrospective Case control study was conducted among 180 patients who undergone pneumonectomy and minimal Lung resection. Data was collected using checklist by trained data collectors. The collected data was entered and analyzed using Statistical Package for social science (SPSS V.25). Univarate, bi-variable and multi-variable analysis were applied to answer the objectives. The Pearson’s chi-square test, COR and AOR were calculated for categorical variables, where appropriate. To identify factors associated with pneumonectomy, binary logistic regression model were computed and Odds Ratio with 95% confidence interval were calculated. A p-value of < 0.25 was used as a cut off points in the crude association to include in to the multivariate analysis. Finally, a p-value of < 0.05 was used to declare significance in the final model.
Results: The majority of patients are in the age range of 20-30s, 27 (48.2%) for the pneumonectomy and 41 (33.1%) for the MLR with male to female ration of 1.6:1 and 1.3:1 in pneumonectomy and MLR respectively. 62.5% (35) of the pneumonectomy and 41.9% (52) of the MLR the patient operated for inflammatory conditions while 32.1% (18) of the pneumonectomy and 33.1% (41) of the MLR Carcinoid tumor is the surgical indication whereas Lung Ca is the diagnosis for 5.4% (3) of pneumonectomy and 25.0% (31) for MLR. Emergency admission (AOR, 3.43; 95%CI: 1.28, 8.67), Tb treatment history (AOR, 40.3; 95%CI: 3.01, 540.2), intra operative blood loss > 500ml (AOR, 9.07; 95%CI: 1.04, 79.13), and post-operative complication (AOR, 37.9; 95%CI: 1.82, 792) were identified as associated factors with pneumonectomy. The postoperative complication rate is 25% and 12.1% in pneumonectomy and MLR respectively whereas the mortality is 5.4% and 2.4% in pneumonectomy and MLR respectively.
Conclusion and Recommendations: Pneumonectomy is commonly performed for inflammatory conditions in TASH. Emergency admission, Tb treatment history, blood loss, and post-operative complication factors significantly associated with pneumonectomy. Tb prevention, screening strategy and proper patient evaluation and diagnosis before starting on treatment should get an attention at all health facility level.
KEYWORDS
Pneumonectomy; Minimal Lung Resection; Associated Factors; Short Term Outco.
INTRODUCTION
Background
In 1933 by Evarts A. Graham performed the first pneumonectomy for 48 years old obstetrician who survived longer for lung carcinoma. Sarot described the first extrapleural pneumonectomy in 1949, which was initially used for TB empyema treatment but later became more commonly used for mesothelioma treatment [1].
Pneumonectomy is a valuable surgical option for anatomically resectable non-small cell lung cancer when other lesser resection will not clear the tumor and pneumoncetomy for inflammatory lung condition is usually associated with tuberculosis but it is associated with significant morbidity and mortality. There is no clear finding which shows the important risk factors for poor outcome. Preoperative assessment is important to identify high risk patients, and adequate pre-operative and operative cover with anti-tuberculosis drugs may enhance results [1-5].
Pneumonectomy is a procedure used to treat a wide variety of nonmalignant diseases of the lung. It is important to treat underlying infections prior to surgery to minimize sputum production, improve nutritional status, decrease chance of intra operative spillage, and decrease postoperative bronchopleural fistulas. Despite the challenges of performing a pneumonectomy for inflammatory diseases, cure rates for MDR-TB, MOTT infections, and fungal disease are excellent. Pneumonectomy for trauma is associated with very high mortality, and efforts should be made to avoid it if possible. Pneumonectomy for other benign conditions is uncommon. Low albumin levels increased the risk of developing postoperative complications in patients who were performed surgical resection for destroyed lung. Pneumonectomy should not be avoided as surgical treatment in eligible patients with destroyed lung [6,7].
Extrapleural Pneumonectomy (EPP) is a technically demanding operation. Right pneumonectomy is associated with a higher mortality due to the increased risk of bronchopleural fistula on the right. peri-operative transfusion, respiratory infection at the time of presentation, neoadjuvant therapy, right-sided pneumonectomy, manual type of bronchial closure, days of postoperative hospitalization and mechanical ventilation as significant risk factors for BPF development. A stump coverage policy showed a low incidence of BPF development, but mechanical stapling was superior to manual closure. Early recognition of possible risk factors associated with fistula development is of paramount importance [8-10].
Bronchial stump closures are a conflicting idea in literature, with some suggesting reinforcement with a pericardial flap to prevent postpneumonectomy bronchopleural fistula, while other studies found no significant impact on the occurrence of BPF. Some literature also showed only right-sided pneumonectomy was associated with higher BPF occurrence than the closure techniques [11,12].
Statement of the Problem
Pneumonectomy has the highest mortality rate among lung resections, with limited literature distinguishing predictors of post pneumonectomy in-hospital mortality from early post discharge mortality. It is associated with a patient suffering a major complication, such as treated cardiac arrhythmias, unplanned intensive care admissions, further surgery, inotrope usage, or 30 day mortality. A careful preoperative physiologic assessment is useful for identifying those patients at increased risk and enabling an informed decision about the appropriate therapeutic approach to treating lung cancer [1-4].
The altered postoperative physiology after pneumonectomy interventions can have severe implications, especially in patients receiving adjuvant therapy for advanced lung cancer. This can lead to cardiovascular and respiratory complications that can increase morbidity and mortality [13]. Pulmonary edema complicating lung resection was first described by Gibbon and Gibbon in 1942. It has since been identified as noncardiogenic pulmonary edema, Acute Lung Injury (ALI), Acute Respiratory Distress Syndrome (ARDS), and Postpneumonectomy Pulmonary Edema (PPE). The main manifestations are increased pulmonary perfusion flow, endothelial damage, and amputation of the lymphatic system. Treatment depends on the physiological situation of the lung remaining after pneumonectomy, and prevention requires co-operation between the medical and surgical teams [14].
Bronchopleural fistula, arrhythmia, cardiac herniation, pulmonary complications, and respiratory failure is a common complication of pneumonectomy [15]. The purpose of this study is to assess factors associated with pneumonectomy and investigate rates of major complications, in-hospital mortality rates, and to compare with other minimal lung resection surgery from a review of patient records.
Objectives
The objective of the study is to identify factors associated with pneumonectomy, its common indication country and its short term outcomes among patients undergone lung resection at TASH from January 2017 to December 2022, Ethiopia which is low and middle income country and stimulate further study in the future.
METHODS
Study Area and period
The study was conducted at Tikur anbessa specialized hospital, Addis Ababa. The research employed the use of this hospital to facilitate the generation of data sufficient to produce accurate and meaningful results that would indicate factors associated with pneumonectomy and short term outcome compared to minimal lung resections. TASH, established in 1972, is a teaching hospital of the AAU, CHS. It is the largest hospital referral hospital in the country with 700 in-patient beds. The thoracic surgery unit has a total of 21beds and with an average of 288 surgeries per year and the only public hospital in the country where major lung resection is performed during the study period. The study was conducted on patients operated for Lung resection from January1, 2017 to December 31, 2022.
Study Design
A 5 years retrospective case control study was conducted using record review of patients operated during the study period.
Source Population
All patients who undergone operations at thoracic Surgery operating room of TASH were the source population for the study.
Study Population
All patients who were operated for pneumonectomy (cases) and Minimal lung resection (Controls) were the study populations.
Inclusion Criteria
All patients who underwent lung resection in TASH during the study period were included.
Exclusion Criteria
Patients with missing information on the indication, outcome or major exposure variables on their medical records and for which secondary data source to identify the missing information cannot be obtained were excluded from the study.
Sample Size Determination
A total of 1207 patients were operated in thoracic surgery operation table during the study period for different thoracic problems of which 61 patients undergone pneumonectomy whereas 128 patients undergone lung resection lesser than pneumonectomy during study period. From these 56 cases for pneumonectomy and 124 for other lung resection (Minimal Lung resection) who fulfil the eligibility criteria were the study sample size.
Preoperative Preparation and Selection for Surgery
Patients with thoracic surgery problem referred to TASH from all over the country either as emergency or cold cases for further evaluation and diagnosis. Patients who referred as an emergency are usually those who present with massive hemoptysis and needs urgent stabilization and intervention. Those patients who are referred as cold cases are evaluated at outpatient department and put on waiting list for surgery and admitted based on their waiting list usually within three month and operated based on the imaging and bronchoscope finding. All patients who admitted for lung resection is based on CT scan finding and the extent of lung damage on CT scan determines the extent of lung resection in our set up. Bronchoscope is usually performed for few patients as we don’t have expertise in this area and patients with clear centrally located tumor for which bronchoscopic biopsy needed.
Patients usually undergone basic laboratory tests and physical perform status assessment is using climb of stare and those who climb 5 stairs are a candidate for pneumonectomy and those who climb at least 2 fight of stares can undergo lung resection lesser than pneumonectomy in our setup since we don’t usually do spirometric and other pulmonary tests. For patients who are older than 45 years of we usually perform Echocardiography as part of cardiac assessment and if they have major structural and functional abnormality we exclude it from surgery.
SURGICAL TECHNIQUES
Posteriolateral thoracotomy is the standard surgical approach for any lung resection and we usually give prophylaxis antibiotics after induction in our set. Extrapleural pneumonectomy is usually performed for patients who have significant inflammatory adhesion between parietal and visceral pleura and access to the hilum is difficult. Usually close the bronchial set with hand sewing using non absorbable suture with two layers and sometimes cover the stump with tissues based on the stump status and surgeons prefererances. We always put chest tube at the end of the procedures and remove on first post-operative day for pneumonectomy and based on output and lung expansion for other minimal lung resections.
Study Variables
Outcome Variables:Improvement, Same/complicated, Death.
Exposure Variables
- Socio-demographic characteristics; age, sex.
- Preoperative parameters/clinical parameters; Duration of symptoms, presenting symptoms, etiology (diagnosis), comorbidities, smoking, TB treatment history, emergency or elective admission .
- Intraoperative Parameters; Pneumonectomy Side (right/left), Type of procedure (intrapleural,extrapleural, intrapericardial completion, lobectomy, lobectomy, segmentectomy and wedge resection), Duration of surgery, Intra OP blood loss, Intra op incident.
- Post-operative parameters; Need for post op ventilation, Need for inotropes, Need for ICU admission, and Length of post op hospital stay.
Data Collection Procedures
Data was collected from patients’ medical record using a data abstraction tool (checklist) that consists of all the variables by trained data collectors. Two residents were recruited and given one day training on how to collect the necessary information. The recorded data includes sociodemographic characteristics, preoperative characteristics, intra and postoperative characteristics.
Quality Assurance
To see the appropriateness of the checklist 10 medical charts were randomly selected for the pretest and the necessary revision on the data collection tool was made based on the test result. The data collectors were supervised by the principal investigator during data collection.
Data Management and Analysis
The collected data was cleaned and entered in to statistical package for social science version 25 for its management and analysis. Univarate, bi-variable and multi-variable analysis were computed to answer the objectives. Principally binary logistic model was used to compare the associations between the study variables and predict for the population parameters. To compare the pneumonectomy and MLR group crosstab descriptive analysis was done with p value < 0.25 was considered as a cut off points to include in to multivariate model.
To compare the underlying socio-demographic and clinical characteristics and operative parameters between pneumonectomy and MLR, a chi-square test, COR and AOR with its 95% CI was run after testing the assumptions for each of these tests. Statistically significant difference was declared at a p-value of < 0.05. Finally the results were summarized and presented using tables and charts.
ETHICAL CONSIDERATION
Before data collection ethical approval was obtained from the Research Ethical of Committee of surgery Department/IRB of AAU, CHS. As a routine procedure, all patients coming to the operation theatre to undergo a major surgery at the hospital give oral and written informed consent which also declares the intraoperative findings and samples will be used for academic and research purposes when needed. Hence, consent was already secured. Medical record number was used for the data collection and personal identifier of the patient was not used in the research report. Access to the collected information was limited to the principal investigator and confidentiality was maintained throughout the project.
RESULTS
Socio-Demographic Characteristics of the Study Subjects
In this study a total of 56 cases and 124 controls were included. The majority of the study subjects were within the age groups of 21 to 30 years which is 42.8% for cases and 33.1% for controls. The mean (+SD) of the study subjects was 36.66 (+/- 14.78) years. Mostly males were operated for Lung resection surgery 62.5% for cases and 56.5% for controls (Table 1).
Table 1 :Socio-demographic characteristics of the study subjects who undergone lung resection at TASH from January 2017 to December 2022.
|
Variables |
Response category |
Cases |
Controls |
|
Number (%) |
Number (%) |
||
|
Age in yrs. |
10-20 |
4 (7.1) |
8 (6.5) |
|
21-30 |
27 (48.2) |
41 (33.1) |
|
|
31-40 |
12 (21.4) |
28 (22.6) |
|
|
41-50 |
6 (10.7) |
16 (12.9) |
|
|
51-60 |
5 (8.9) |
21 (16.9) |
|
|
61 and above |
2 (3.6) |
10 (8.1) |
|
|
Sex |
Male |
35 (62.5) |
70 (56.5) |
|
Female |
21 (37.5) |
54 (43.5) |
Clinical Characteristics of the Study Subjects
About 80.4% (45) of the pneumonectomy and 92.7% (115) of the MLR groups admitted on elective bases while 19.6% (11) of the case and 7.3% (9) of the control groups with p value of 0.01, are admitted on emergency but operated on elective bases after the patient stabilized. In 67.9% (38) of the pneumonectomy and 71.8% (89) of the MLR group the duration of the symptom is 6weeks and less whereas 32.1% (18) of the pneumonectomy and 28.2 %( 35) of the MLR group the duration of presenting symptoms is above 6 weeks. Also, 92.9% (52) of the pneumonectomy and 96.8% (120) of the MLR group has no history of smoking whereas 7.1% (4) of the pneumonectomy and 3.2% (4) 0f the MLR has history of cigarette smoking.
Moreover, 75.0% (42) of the pneumonectomy and 19.4% (24) of the MLR group has history of Tb treatment Whereas 25.0 %( 14) of the Pneumonectomy and 80.6% (100) of the MLR has no history of Tb treatment with P value of < 0.01 which indicated TB has high association for the pneumonectomy case. For 12.5% (7) of patients the pneumonectomy is unplanned preoperatively whereas 87.5% (49) the pneumonectomy is a planned surgery. Also, 55.4% (31) of the pneumonectomy and 44.4% (55) of MLR is on left side while 44.6% (25) of the pneumonectomy and 55.6% (69) of MLR is on the right side. (Table 2).
Table 2: Clinical characteristics of the study subjects who undergone lung resection at TASH from January 2017 to December 2022.
|
Variables |
Response category |
Cases |
Controls |
P value |
|
Number (%) |
Number (%) |
|||
|
Admission |
Elective |
45 (80.4) |
115 (92.7) |
0.01 |
|
Emergency |
11 (19.6) |
9 (7.3) |
||
|
Duration of symptom presentation >6weeks |
No |
38 (67.9) |
89 (71.8) |
0.56 |
|
Yes |
18 (32.1) |
35 (28.2) |
||
|
History of smoking |
No |
52 (92.9) |
120 (96.8) |
0.24 |
|
Yes |
4 (7.1) |
4 (3.2) |
||
|
History of TB |
No |
14 (25.0) |
100 (80.6) |
<0.01 |
|
Yes |
42 (75.0) |
24 (19.4) |
||
|
Comorbid illness |
No |
52 (92.9) |
114 (91.9) |
0.46 |
|
Yes |
4 (7.1) |
10 (8.1) |
|
|
|
Side of lung resection |
Left |
31 (55.4) |
55 (44.4) |
|
|
Right |
25 (44.6) |
69 (55.6) |
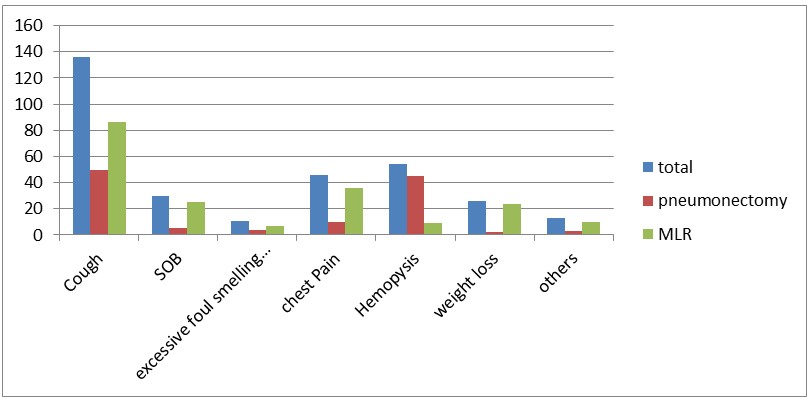
Figure 1: Presenting symptoms of the study subjects whom undergone lung resection at TASH from January 2017 to December 2022 N.B the total symptom may not =100% since one patient may have more than one symptoms.
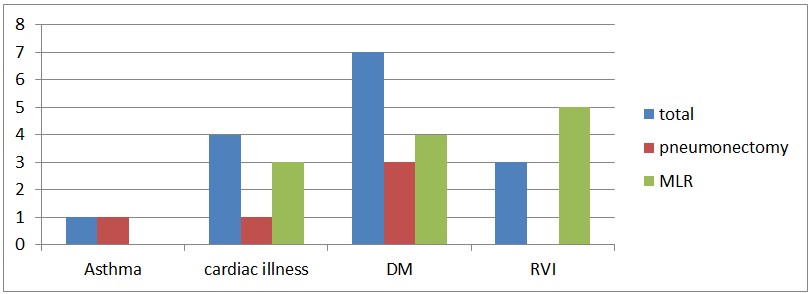
Figure 2: Comorbidities of patients who operated for lung resection in TASH from January 2017 to December 2022.
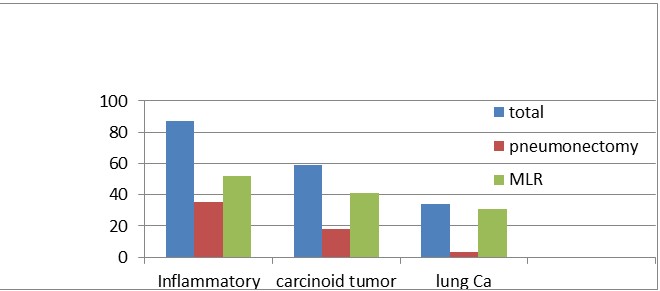
Figure 3: Surgical indication of the study subject who undergo lung resection in TASH from January 2017 to December 2022.
From the result, most, 89.29% (50) of pneumonectomy and 69.35% (86) of MLR group cough is the presenting symptom while 8.93% (5) of the pnemonectomy and 20.16% (25) of MLR group SOB is the presenting symptom whereas excessive foul smelling sputum present 7.14% (4) in pneumonectomy and 5.64% (7) in MLR, while chest pain is the presenting symptom in 17.86% (10) in pneumonectomy and 29.03% (8) the MLR group, 80.34% (45) of the pneumonectomy and 7.23% (9) of MLR hemoptysis is the presenting symptom in whereas 3.57% (2) of the pneumonectomy and 19.35% (24) of the MLR patients present with weight loss and 5.36% (3) of the pneumonectomy and 8.10% (10) of MLR present with other symptoms (Figure 1).
From the 7.1% (4) of the pneumonectomy and 8.1% (10) of the MLR group who has comorbid illness; Asthma 1.8% (1), Cardiac illness 1.8% (1), DM 3.6% (2) is found in the pneumonectomy whereas cardiac illness 2.4% (3), DM 2.4% (4) and RVI 2.4% (3) in the MLR group are the comorbid illness (Figure 2).
Also, from the findings, 62.5% (35) of the pneumonectomy and 41.9% (52) of the MLR the patient operated for inflammatory conditions(post Tb complications like Aspergilloma, bronchiectasis lung fibrosis, bleeding from cavitary lesions, extensive bullous diseases) while 32.1% (18) of the pneumonectomy and 33.1% (41) of the MLR Carcinoid tumor is the surgical indication whereas non-small cell lung Cancer is the diagnosis for 5.4% (3) for the pneumonectomy and 25.0% (31) for the MLR (Figure 3).
Intra and Postoperative Characteristics of the Study Subject
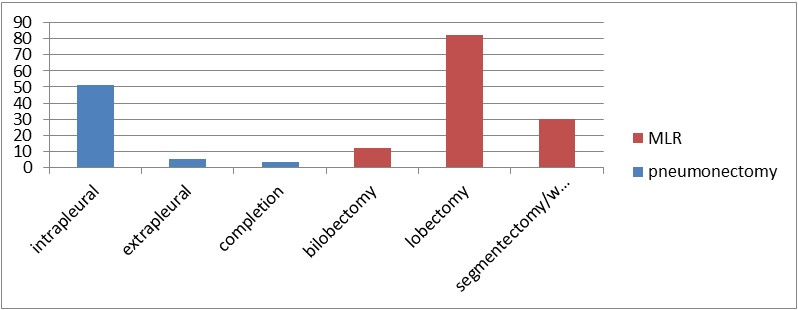
The result also showed about 91.1% (51) of the procedure is an intrapleural, 8.9% (5) an extrapleural, 5.4% (3) is a completion pneumonectomy whereas 66.1% (82) is lobectomy, 9.7% (12) is bilobectomy and 24.2% (30) is segmentectomy and wedge resection are procedures performed for the MLR group (Figure 4).
Figure 4: Surgical procedures for who undergone lung resection patients in TASH from January 2017 to December 2022.
Figure 5: Surgical procedures for who undergone lung resection patients in TASH from January 2017 to December 2022.
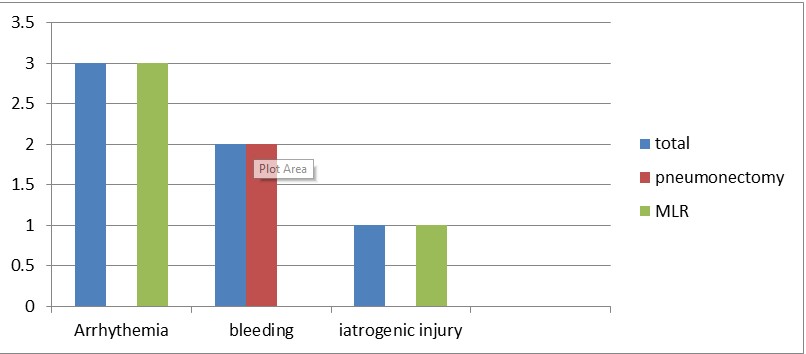
From the result, 82.1% (46) of the pneumonectomy and 30.6% (38) of the MLR, the estimated blood loss is greater than 500ml with p value < 0.01. In addition87.5% (49) of pneumonectomy and 58.1% (72) of the MRL the operative time is greater than 180 minutes with P values < 0.01. 3.6% (2) of pneumonectomy and 3.2% (4) of MLR has intraoperative incident. Moreover 12.5% (7) of the pneumonectomy and 10.5% (13) of the MLR require inotropes in the immediate post-operative period. Whereas 1.8% (1) of the pneumonectomy and 5.6% (7) of the MLR require postoperative positive ventilation (Table 3). Bleeding occur in 3.6% ( 2) in the pneumonectomy group intraoperative whereas Arrhythmia 2.4 % (3) and iatrogenic injury to nearby structure 2.4% (1) occurs in the MLR group (Figure 5). 23.2% (13) of pneumonectomy and 40.3% (50) of MLR stay in the hospital more than 7 days (Table 3).
Table 3: intra and postoperative parameters of the study subjects who undergone lung resection in TASH from January 2017 to December 2022.
|
Variables |
Response category |
Cases |
Controls |
P value |
|
Number (%) |
Number (%) |
|||
|
Duration of surgery > 180 minute |
No |
7 (12.5) |
52 (41.9) |
<0.01 |
|
Yes |
49 (87.5) |
72 (58.1) |
||
|
Blood loss > 500ml |
No |
7 (12.5) |
72 (58.1) |
<0.01 |
|
Yes |
49 (87.5) |
52 (41.1) |
||
|
Intraoperative incident |
No |
54 (96.4) |
120 (96.8) |
0.23 |
|
Yes |
2 (3.6) |
4 (3.2) |
||
|
Post op inotropes |
No |
49 (87.5) |
111 (89.5) |
0.69 |
|
Yes |
7 (12.5) |
13 (10.5) |
||
|
Post Op positive ventilation |
No |
55 (98.2) |
117 (94.4) |
0.02 |
|
Yes |
1 (1.8) |
7 (5.6) |
||
|
Post Op Complication |
No |
42 (75.0) |
109 (87.9) |
0.03 |
|
Yes |
14 (25.0) |
15 (12.1) |
||
|
Hospital stay >7 days |
No |
43 (66.8) |
74 (59.7) |
0.03 |
|
Yes |
13 (23.2) |
50 (40.3) |
Outcomes of Lung Resection
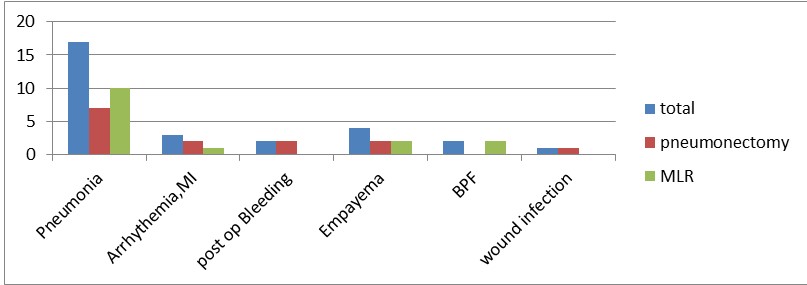
25.0% (14) of the pneumonectomy and 12.1% (15) of the MLR develop post op complication with p value of 0.03 which shows post-operative complication occurs more common in the pneumonectomy group (Table 3). Among the complications Arrhythmia and MI 3.6% (2) in the pneumonectomy and 0.8% (1) MLR, postop bleeding 3.5% (2) in the Pneumonectomy, BPF 1.6% (2) in the MLR group, Empyema 3.6% (2) in the pneumonectomy and 1.6% (2) in the MLR, Pneumonia 12.5% (7) in the pneumonectomy and 8.1% (10) in the MLR and wound infection1.8% (1) in the pneumonectomy group are occurred (Figure 7,6).
Figure 6: Post op complications in patients who undergone lung resection in TASH from January 2017 to December 2022.
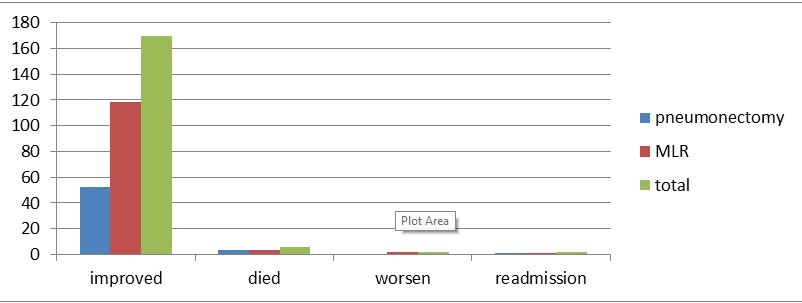
Figure 7: Outcomes of Pneumonectomy among the study subjects whom undergone lung surgery at TASH from January 2017 to December 2022.
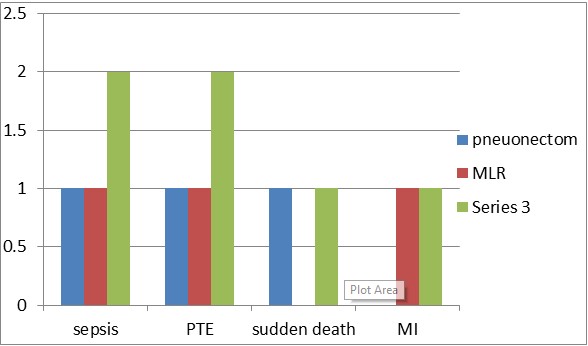
The majority, 92.9% (52) of the pneumonectomy and 95.2% (118) of the MLR discharged improved while 5.4% (3) of the pneumonectomy and 2.4% (3) of the MLR died whereas 1.6% (2) of the MLR worsen from admission time whereas 1.8% (1) of the pneumonectomy and 0.8% (1) of the MLR group readmitted within one month duration (Figure 7). Among the death, Sepsis 33.3% (1), PTE 33.3% (1) in both groups and sudden death 33.1% (1) in pneumonectomy and MI 33.1% (1) in MLR group is the probable cause of death (Figure 8).
Factors Associated with Pneumonectomy Compared to MLR
On the final model variables like admission, Tb treatment history, estimated intra operative blood loss > 500ml, and post-operative complications are significantly associated with Pneumonectomy (P < 0.05). Accordingly, those patients admitted on Emergency were more (AOR, 3.43; 95%CI: 1.28, 8.67) likely to undergo pneumonectomy than minimal lung resection compared to those admitted with elective. This is may be because his patients are presented with massive hemoptysis and extensive underlying lung damage. Also, patients with no previous history of Tb treatment are more (AOR, 40.3; 95%CI: 3.01, 540.2) likely to undergo minimal lung resection than pneumonectomy. there is two explanation for this reason : one is patients who wrongly diagnosed as Tb while they have endobroncheal tumors will progress to obstructive bronchiectasis and permenant lung damage end up with pneumonectomy till they complete anti Tb drugs and referred after they get complicated and the second reason is patient who have real tuberculosis was not get proper medical treatment and get complicated and end up with pneumonectomy. For those study subjects having an EBL > 500ml were more (AOR, 9.07; 95%CI: 1.04, 79.13) likely associated with pneumonectomy compared to their counterparts. In addition, patients who had Post Op complications were (AOR, 37.9; 95%CI (1.82, 792.3) is likely associated pneumonectomy (Table 4).
DISCUSSION
The earliest successful pneumonectomies were performed for suppurative lung disease. At present time pneumonectomy is reserved for patients whose cancer requires complete pneumonectomy for cure and only for selected suppurative lung disease. It is usually reserved for patients with more advanced disease when the tumor is located in the main stem bronchus or extends across major fissure. Non-small cell lung cancer lung cancer is the most common type of malignancy requiring pneumonectomy. It is sometimes also indicated for mesotheliomas and extensive tumors from adjacent structure like thymus [1-30].
Figure 8: Causes of death among patients undergone lung resection in TASH from January 2017 to December 2022.
Table 4: Factors Associated with pneumonectomy among the study subjects who undergone lung resection at TASH from January 2017 to December 2022.
|
Variables |
Pneumonectomy |
COR (95% CI) |
AOR (95%CI) |
P value |
|
|
Yes |
No |
||||
|
Number (%) |
Number (%) |
||||
|
Admission |
|||||
|
Elective |
55 (80.4%) |
115 (92.7%) |
1 |
0.02 |
|
|
Emergency |
11 (19.6%) |
9 (7.3%) |
3.13 (1.21,8.04) |
3.43 (1.28, 8.67) |
|
|
History of Tb RX |
|||||
|
Yes |
42 (75.0%) |
24 (19.4%) |
1 |
0.02 |
|
|
No |
14 (25.0%) |
100 (80.6%) |
12.5 (5.89,26.16) |
40.3 (3.01,540.2) |
|
|
EBL > 500ml |
|||||
|
Yes |
49 (82.1%) |
72 (30.6%) |
1 |
0.002 |
|
|
No |
7 (17.9%) |
52 (69.4%) |
10.4 (4.75,78) |
9.07 (1.04,79.13) |
|
|
Post Op CXN |
|||||
|
Yes |
14 (25.0%) |
15 (12.1%) |
1 |
0.02 |
|
|
No |
42 (75.0%) |
109 (87.9) |
2.4 (1.18,5.92) |
37.9 (1.82,792.3) |
|
Among the most common nonmalignant conditions which require pneumonectomy is inflammatory lung disease which includes post Tb bronchoectais, Aspergilloma with massive hemoptysis, lung fibrosis, extensive bullous disease and cavitary lesions). Such group of patients should be properly optimized before surgery with medical treatment of underlying infections, optimization of lung functions and patients nutrition [5-30].
The study included 56 pneumonectomy patients and 124 other lung resection patients, with a median age of 35 years and a male predominance (58.3%). The most common symptom presentation is cough 89.2% for pneumonectomy and 69.35% for MLR whereas hemoptysis is far common in pneumonectomy (80.34%) and 7.23% in MLR. TB treatment history is the most common in the pneumonectomy (75%) whereas only 19.4% in MLR patients. In our study Lung resection is indicated mainly for inflammatory conditions (post TB complicatios (62.5%) for pneumonectomy and (41.9%) for MLR. A 1979 retrospective study conducted in Nigeria university hospital shows pneumonectomy mostly performed for life treating hemorrhage post Tb destroyed lung and a study from university of Natan medical school, South Africa (2000) shows 72% of pneumonectomy is associated with Tb where as a prospective study from UK 2009 and a retrospective study at Al Hussein teaching hospital from Baghdad in 2022 shows pneumonectomy is indicated for lung Ca [1-28].
This study demonstrated that pneumonectomy is associated with among emergency admission (19.6% vs 7.3%), previous Tb treatment history (75% vs 19.4%), greater intraoperative blood loss (87.5% vs 58.5%) and higher post-operative complication rate (25% vs 12.1%) compared to those patients who undergone minimal lung resection. This research result also shows shorter length of hospital stay (76.8% vs 59.7%) in pneumonectomy, whereas the hospital mortality rate higher (5.4% vs 2.4%) but statistically no significant difference with minimal lung resection group.
The complications of pneumonectomy in our study shows pneumonia 12.5%, arrhythmia 3.6%, post op bleeding 3.6%, Empyema 3.6% and wound infection 1.8% whereas arrhythmia 0.8%, BPF 1.6%, empyema 1.6% and pneumonia 8.1% are post op complications in MLR patients. In study from University of Natan medical school(2000) shows morbidity rate of 23% closer to this study and Empyema(14.8), bleeding (1.9), BPF (1.9) and wound sepsis (0.6) whereas study from Baghdad shows arrhythmia and atelectasis 40% and UK 19.9% in pneumonectomy is which higher than our study [1-28].
Pneumonectomy has the highest mortality rate among resections. Mortality rate is 5.4% in our study whereas 1.2% from South Africa, 25% from Nigerian study, 5.4% from UK and 3% from Baghdad study. This study shows even if most of the pneumonectomy indication in our set up is benign disease in which mortality is higher, the mortality rate in our set up is comparable with a malignant indication of pneumonectomy [1-30].
One of the main limitations of this research is, since it is retrospective study, tracing patient a patient record was challenging and some of the patient was excluded from the study. On the other hand important patient information like (ASA, performance status, and bronchial closure technique) is not recorded on the chart and this limits to analyze the factors associated with outcome of pneumonectomy [1-34].
CONCLUSION AND RECOMMENDATIONS
Conclusion
Pneumonectomy in TASH is commonly done for inflammatory condition mostly associated with TB. Emergency admission and hospital stay. This study shows that pneumonectomy in particular and lung resection in general is usually indicated for benign condition in our set in contrast the study done in developed country. Pneumonectomy is also associated with high morbidity rate and comparable mortality rate with other minimal lung resection and the finding is almost comparable with the literature’s which done in best setup. So any lung resection in our set up can be performed safely without more harmful to the patient.
Recommendation
Since pneumonectomy is associated with Tb treatment history either directly by destroying lung or indirectly patients wrongly started on anti TB resulting in lung damage from delay treatment which can be managed by without resection or minimal resection, Tb prevention strategy and proper patient evaluation and diagnosis before treatment should get an attention at all health facility level in order to limit the extent of lung damage and safe the patient from undergoing major Lung resection.
ACKNOWLEDGMENT
We would like thank you that assisted in data collection, typing the manuscript and also who advised us on statistical analysis of the result. We would also like thank Addis Ababa university Department of surgery IRB.
REFERENCES
- Powell ES, Pearce AC, Cook D, Davies P, Bishay E, Bowler GM, et al. UKPOS Co-ordinators. UK pneumonectomy outcome study (UKPOS): a prospective observational study of pneumonectomy outcome. J Cardiothorac Surg. 2009; 4: 41. doi: 10.1186/1749-8090-4-41. PMID: 19643006; PMCID: PMC2726136.
- Beshara M, Bora V. Pneumonectomy. [Updated 2022 Sep 18]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022
- Ali Al-Ghuzey, Ahmed Abdulameer Daffar, Rafid Remthan Hussein Al-Temimi, Enass Mahdi saleh, Halah Ghalib. A retrospective study of pneumonectomy: Review of 100 cases in Al-Hussein teaching hospital/Thi-Qar (2013-2020). Curr Pediatr Res. 2022; 26: 1427-1432.
- Brunelli A, Kim AW, Berger KI, Addrizzo-Harris DJ. Physiologic evaluation of the patient with lung cancer being considered for resectional surgery: Diagnosis and management of lung cancer, 3rd ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest. 2013; 143: e166S-e190S. doi: 10.1378/chest.12-2395. Erratum in: Chest. 2014 Feb;145(2):437. PMID: 23649437.
- Blyth DF. Pneumonectomy for inflammatory lung disease. Eur J Cardiothorac Surg. 2000; 18: 429-434. doi: 10.1016/s1010-7940(00)00526-1. PMID: 11024380.
- Conlan AA, Kopec SE. Indications for pneumonectomy. Pneumonectomy for benign disease. Chest Surg Clin N Am. 1999; 9: 311-326. PMID: 10365265.
- Kosif M?s?rl?o?lu A, Bayram S, K?ral H, Çoban A?ca M, Tokgöz Aky?l F, Alpay L, et al . Factors affecting complication rates of pneumonectomy in destroyed lung. Turk Gogus Kalp Damar Cerrahisi Derg. 2018; 26: 272-278. doi: 10.5606/tgkdc.dergisi.2018.14635. PMID: 32082745; PMCID: PMC7024126.
- Zellos L, Jaklitsch MT, Al-Mourgi MA, Sugarbaker DJ. Complications of extrapleural pneumonectomy. Semin Thorac Cardiovasc Surg. 2007; 19: 355-359. doi: 10.1053/j.semtcvs.2008.01.001. PMID: 18395638.
- Darling GE, Abdurahman A, Yi QL, Johnston M, Waddell TK, Pierre A, et al . Risk of a right pneumonectomy: role of bronchopleural fistula. Ann Thorac Surg. 2005; 79: 433-437. doi: 10.1016/j.athoracsur.2004.07.009. PMID: 15680809.
- Panagopoulos ND, Apostolakis E, Koletsis E, Prokakis C, Hountis P, Sakellaropoulos G, et al. Low incidence of bronchopleural fistula after pneumonectomy for lung cancer. Interact Cardiovasc Thorac Surg. 2009; 9: 571-575. doi: 10.1510/icvts.2009.203646. Epub 2009 Jul 14. PMID: 19602497.
- Taghavi S, Marta GM, Lang G, Seebacher G, Winkler G, Schmid K, et al. Bronchial stump coverage with a pedicled pericardial flap: an effective method for prevention of postpneumonectomy bronchopleural fistula. Ann Thorac Surg. 2005; 79: 284-288. doi: 10.1016/j.athoracsur.2004.06.108. PMID: 15620959.
- Skrzypczak P, Roszak M, Kasprzyk M, Dyszkiewicz W, Kami?ski M, Gabryel P, et al. The technique of stump closure has no impact on post-pneumonectomy bronchopleural fistula in the non-small cell lung cancer-a cross-sectional study. J Thorac Dis. 2022; 14: 3343-3351. doi: 10.21037/jtd-22-240. PMID: 36245618; PMCID: PMC9562551.
- Piraccini E, Agnoletti V, Corso RM, Chanis-Vargas J, Gaetani S, Gambale G. Left diaphragmatic hernia after pneumonectomy. HSR Proc Intensive Care Cardiovasc Anesth. 2010; 2: 299-300. PMID: 23439328; PMCID: PMC3484592.
- Tsukada G, Stark P. Postpneumonectomy complications. AJR Am J Roentgenol. 1997; 169: 1363-1370. doi: 10.2214/ajr.169.5.9353460. PMID: 9353460.
- Faisy C, Bazelly B, Saïdi F, Lafon B, Tordjman R, Parrot A. Cedème pulmonaire postpneumonectomie. Revue de la littérature. A propos de deux nouveaux cas [Postpneumonectomy pulmonary edema. Review of the literature. Apropos of 2 new cases]. Rev Pneumol Clin. 1996; 52: 253-260. French. PMID: 9033924.
- Abbas Ael-S, Deschamps C. Postpneumonectomy empyema. Curr Opin Pulm Med. 2002; 8: 327-333. doi: 10.1097/00063198-200207000-00015. PMID: 12055398.
- Vallieres E, Shamji FM, Todd TR. Postpneumonectomy chylothorax. Ann Thorac Surg. 1999; 55: 1006-1008. doi: 10.1016/0003-4975(93)90138-8. PMID: 8385443.
- Bédard EL, Uy K, Keshavjee S. Postpneumonectomy syndrome: a spectrum of clinical presentations. Ann Thorac Surg. 2007; 83: 1185-1188. doi: 10.1016/j.athoracsur.2006.08.021. PMID: 17307492.
- Zwischenberger JB, Alpard SK, Bidani A. Early complications. Respiratory failure. Chest Surg Clin N Am. 1999; 9: 543-564, viii. PMID: 10459429.
- Ferretti G, Brichon P, Jankowski A, Coulomb M. Imagerie des complications survenant après chirurgie de résection pulmonaire [Postoperative complications after thoracic surgery]. J Radiol. 2009; 90: 1001-1012. French. doi: 10.1016/s0221-0363(09)73238-x. PMID: 19752837.
- Cariati A, Piromalli E, Taviani M. Postpneumonectomy bronchial stump recurrence and bronchopleural fistula. Asian Cardiovasc Thorac Ann. 2012; 20: 439-442. doi: 10.1177/0218492312445588. PMID: 22879551.
- Deschamps C, Pairolero PC, Allen MS, Trastek VF. Management of postpneumonectomy empyema and bronchopleural fistula. Chest Surg Clin N Am. 1996; 6: 519-527. PMID: 8818419.
- Asamura H. Early complications. Cardiac complications. Chest Surg Clin N Am. 1999; 9: 527-541, vii-viii. PMID: 10459428.
- Mammana M, Marulli G, Zuin A, Perissinotto E, Comacchio GM, De Franceschi E, Rea F. Postpneumonectomy bronchopleural fistula: analysis of risk factors and the role of bronchial stump coverage. Surg Today. 2020; 50: 114-122. doi: 10.1007/s00595-019-01871-0. Epub 2019 Sep 6. PMID: 31493198.
- Schneider L, Farrokhyar F, Schieman C, Shargall Y, D'Souza J, Camposilvan I, et al. Pneumonectomy: the burden of death after discharge and predictors of surgical mortality. Ann Thorac Surg. 2014; 98: 1976-1981; discussion 1981-2. doi: 10.1016/j.athoracsur.2014.06.068. Epub 2014 Oct 3. PMID: 25282164.
- Wang H, Wang Z, Zhou M, Chen J, Yao F, Zhao L, et al. Postoperative atrial fibrillation in pneumonectomy for primary lung cancer. J Thorac Dis. 2021; 13: 789-802. doi: 10.21037/jtd-20-1717. PMID: 33717552; PMCID: PMC7947480.
- Owen RM, Force SD, Pickens A, Mansour KA, Miller DL, Fernandez FG. Pneumonectomy for benign disease: analysis of the early and late outcomes. Eur J Cardiothorac Surg. 2013; 43: 312-317. doi: 10.1093/ejcts/ezs284. Epub 2012 May 18. PMID: 22611143.
- Adebonojo SA, Osinowo O, Adebo OA. Pneumonectomy in Nigeria: indications and results. J Natl Med Assoc. 1979; 71: 1077-1080. PMID: 529307; PMCID: PMC2537534.
- James TW, Faber LP. Indications for pneumonectomy. Pneumonectomy for malignant disease. Chest Surg Clin N Am. 1999; 9: 291-309, ix. PMID: 10365264.
- Harvey JC, Erdman C, Beattie EJ. Pneumonectomy. Chest Surg Clin N Am. 1995; 5: 253-287. PMID: 7613964.
- Rusch VW. Indications for pneumonectomy. Extrapleural pneumonectomy. Chest Surg Clin N Am. 1999; 9: 327-338, x. PMID: 10365266.
- Rivera C, Arame A, Pricopi C, Riquet M, Mangiameli G, Abdennadher M, et al . Pneumonectomy for benign disease: indications and postoperative outcomes, a nationwide study. Eur J Cardiothorac Surg. 2015; 48: 435-440; discussion 440. doi: 10.1093/ejcts/ezu439. Epub 2014 Nov 20. PMID: 25414429.
- Al-Kattan K, Goldstraw P. Completion pneumonectomy: indications and outcome. J Thorac Cardiovasc Surg. 1995; 110: 1125-1129. doi: 10.1016/s0022-5223(05)80182-5. PMID: 7475141.
- Villeneuve PJ, Sundaresan S. Complications of pulmonary resection: postpneumonectomy pulmonary edema and postpneumonectomy syndrome. Thorac Surg Clin. 2006; 16: 223-234. doi: 10.1016/j.thorsurg.2006.05.001. PMID: 17004550.