Medium Abundance Hemoptysis Revealing a False Rasmussen
- 1. Department of Pneumology, IBN ROCHD University Hospital Center, Morocco
ABSTRACT
Rasmussen’s aneurysm is a false inflammatory aneurysm of a branch of the pulmonary artery within or adjacent to a tuberculous cavern or other excavated lung lesion, whose rupture may lead to massive hemoptysis.
Our patient, who was at 35 days of antibacillary treatment, complicated by a medium abundance hemoptysis revealing a false Rasmussen’s aneurysm confirmed by chest CT angiography, and treated by embolization of the right inferior lobar artery during a chest angiography. The course was marked by resolution of the hemoptysis.
Rasmussen’s aneurysm remains a rare cause of massive hemoptysis that requires urgent management, relying firstly on endovascular treatment.
KEYWORDS
- Hemoptysis
- Pulmonary tuberculosis
- False aneurysm
- Rasmussen aneurysm
CITATION
Arfaoui H, Bamha H, Nahidi M, Aidou S, Jabri H, et al. (2023) Medium Abundance Hemoptysis Revealing a False Rasmussen’s Aneurysm: A Case Report. Clin Res Pulmonol 9(1): 1054.
INTRODUCTION
Rasmussen’s aneurysm is a peripheral pulmonary artery pseudoaneurysm that occurs due to erosion of a branch of the pulmonary artery near or within a tuberculous cavity [1]. Rupture of a Rasmussen’s aneurysm can cause life-threatening hemoptysis requiring urgent management, making endovascular treatment a recommended treatment modality.
We report the case of a young patient with a Rasmussen’s aneurysm revealed by a medium abundance hemoptysis.
OBSERVATION
A 32 years old male, chronic weaned smoker, under antibacillary treatment for 35 days for pulmonary tuberculosis, without any particular pathological history was admitted in our pneumology department complaining of the occurrence of several episodes of medium abundance hemoptysis , without other thoracic or extrathoracic signs , all evolving in a context of altered general condition and fever.
Respiratory physical examination revealed diffuse snoring in both lungs, oral and urogenital examinations did not reveal any aphthosis or scarring, no pseudo-folliculitis in the skin examination and the PATHERGY-test was negative, the rest of the clinical examination was unremarkable.
The frontal chest X-ray showed an round, inhomogeneous and sharply contoured opacity, with diffuse reticulo-micronodular images and some round excavated opacities (Figure 1).
Figure 1 Frontal chest X-ray.
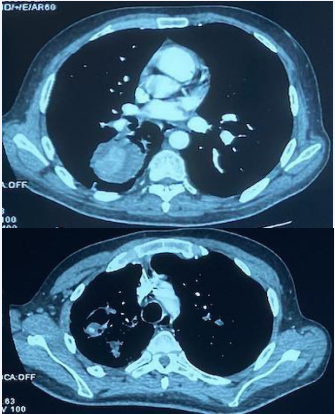
The CT scan showed in the right upper lobar the presence of a hypodense formation with hyperdense center that increased after injection of iodine contrast product , making a vascular pathology suspicious (Figure 2).
Figure 2 CT scan+ PCI injection.
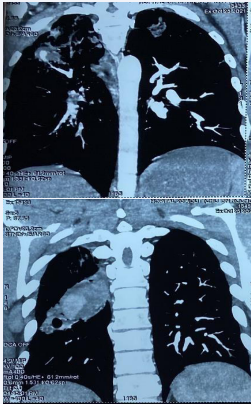
CT angiography showed an aneurysmal dilatation of a sub- segmental pulmonary arterial branch of the dorsal segment of the upper right lobe in favor of a false Rasmussen’s aneurysm with a cavitary lesion of the right Fowler’s vessel with a strongly enhanced area without any communication with a vascular structure complicated by alveolar hemorrhage, multiple cavitary lesions associated with micronodules and mediastinal lymph node involvement of tubercular origin (Figure 3).
Figure 3 CT angiography with reconstruction.
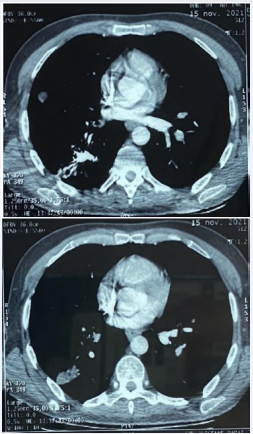
right inferior lobar artery was performed during a pulmonary angiography with first stage puncture of the right femoral artery then catheterization of the right bronchial artery and some right and left intercostal arteries and second stage puncture of the right femoral vein with catheterization of the trunk of the pulmonary artery and its right pulmonary artery with chest CT follow-up (Figure 4).
Figure 4 CT scan after embolization.
Evolution was marked by decreasing of hemoptysis
DISCUSSION
Rasmussen’s aneurysm, named after Fritz Valdemar Rasmussen, is an aneurysm arising from the pulmonary artery proximal to or within a tuberculous cavity.
Although it is reported in 5% of autopsy series of patients with tuberculous caverns, only a few clinical cases exist in the literature [2]. In about 80% of cases, a bronchial or other systemic artery is the source of the bleeding, but in the remaining 20%, a pulmonary artery origin is found [3].
These aneurysms occur in the segmental pulmonary arteries and arise as a result of granulomatous infiltration of the adventitia and media which is replaced over time by fibrin, resulting in thinning of the vessel wall, then the formation of an aneurysm and its rupture causing hemoptysis [4].
Plessinger et al. published a series of 56 cases of Rasmüssen aneurysm in 1956. In 47 cases (87% of total cases), massive pulmonary arterial hemorrhage was responsible for death [5].
This pathology remains responsible for an important mortality due to the severity of the hemoptysis and requires an urgent management.
The injected CT scan is the reference examination to detect the location of the hemoptysis, to specify the vascular mapping, thus allowing an etiological and pathophysiological diagnosis, to guide the clinician on the type of angiography to be performed: either bronchial arteriography or selective pulmonary angiography. This key examination must be strictly protocolized with reconstruction of the native axial views by the radiologist who performs it [6].
Once the diagnosis of aneurysm is made, the management is based on interventional radiology allowing the vaso-occlusion of the pathological artery by pulmonary angiography using microspires (coils), biological glue, detachable balloons, covered stents, or sclerosing agents such as alcohol. Remy et al. have demonstrated that this technique is effective [7,8], but can be accompanied by complications: aneurysmal rupture, pulmonary infarction, gas embolism, anterior spinal branch occlusion [9] while surgical management is accompanied in 50% of cases by postoperative complications and a 20% mortality [10,11].
CONCLUSION
Rasmussen’s aneurysm is a rare and often missed cause of hemoptysis in patients with tuberculous caverns. The injected CT scan remains the best tool for confirmation and should be performed in patients with recurrent hemoptysis. Particular attention should be paid to the embolization of Rasmussen’s aneurysms, as they are very prone to rupture and bleed.
AUTHORS’ CONTRIBUTIONS
All authors contributed to this work. They have read and approved the final version of the manuscript.
PATIENT’S PERSPECTIVE
The patient was satisfied with the diagnostic and therapeutic management.
PATIENT CONSENT
The patient was informed about the study and gave oral consent.
AUTHORS’ CONTRIBUTIONS
All authors approved the final version of the manuscript.
ACKNOWLEDGEMENTS
Les auteurs n’ont aucun remerciement à faire.
REFERENCES
- Chatterjee K, Colaco B, Colaco C, Hellman M, Meena N. Rasmussen’s aneurysm: A forgotten scourge. Respir Med Case Rep. 2015; 16: 74-76.
- Sapra R, Sharma G, Minz AK. Rasmussen’s aneurysm: A rare and forgotten cause of hemoptysis. Indian Heart J. 2015; 67: S53-S56.
- Sanyika C, Corr P, Royston D, Blyth DF. Pulmonary angiography and embolization for severe hemoptysis due to cavitary pulmonary tuberculosis. Cardiovasc Intervent Radiol. 1999; 22: 457-460.
- Giraldo-Montoya ÁM, Rodríguez-Morales AJ, Hernández-Hurtado JD, López-Salazar Á, Lagos-Grisales GJ, Ruiz-Granada VH. Rasmussen aneurysm: A rare but not gone complication of tuberculosis. Int J Infectious Dis. 2018; 69: 8-10.
- Plessinger VA, Jolly PN. Rasmussen’s aneurysms and fatal hemorrhage in pulmonary tuberculosis. Am Rev Tuberc. 1949;60: 589-603.
- Basille D, Andréjak C, Gosset M, Renard C, Jounieaux V. Hémoptysie massive sur anévrisme de Rasmüssen. Revue des Maladies Respiratoires. 2010; 27: 63-66.
- Remy J, Lemaitre L, Lafitte J, Vilain M, Saint Michel J, Steenhouwer F. Massive hemoptysis of pulmonary arterial origin: diagnosis and treatment. Am J Roentgenol. 1984; 143: 963-969.
- Remy-Jardin M, Wattinne L, Remy J. Transcatheter occlusion of pulmonary arterial circulation and collateral supply: failures, incidents, and complications. Radiol. 1991; 180: 699-705.
- Portron Y, Lederlin M, Montaudon M, Corneloup O, Latrabe V, Barbot R, et al. Embolisation d’un faux-anévrysme de Rasmussen compliquant une tuberculose active. J de Radiologie. 2010; 91: 911-914.
- Conlan AA, Hurwitz SS, Krige L, Nicolaou N, Pool R. Massive hemoptysis. Review of 123 cases. J Thorac Cardiovasc Surg. 1983; 85: 120-124.
- McCollum WB, Mattox KL, Guinn GA, Beall AC. Immediate Operative Treatment for Massive Hemoptysis. Chest. 1975; 67: 152-155.