Mucinous Adenocarcinoma mimicking Organizing Pneumonia
- 1. Department of Pulmonary and Critical Care Medicine, Cape Fear Valley Medical Center, USA
- 2. Department of Pathology, Cape Fear Valley Medical Center, USA
Keywords
• Organizing Pneumonia
• Mucinous Adenocarcinoma
Citation
Chapa-Rodriguez A, Harter D, Vaidya1 S, Narechania S (2025) Mucinous Adenocarcinoma mimicking Organizing Pneumonia. Clin Res Pulmonol 11(1): 1075
CASE PRESENTATION
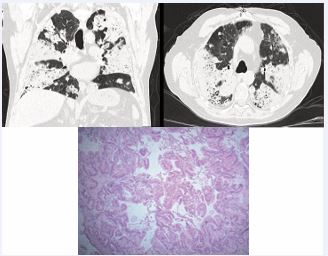
78 year-old man referred to pulmonology for dyspnea, dry cough, and abnormal CT Chest showing consolidative changes in all lobes. Patient had failed multiple antibiotic courses for presumed bacterial pneumonia as well as a steroid course for organizing pneumonia. Infectious and autoimmune work up negative. Given sarcoidosis, organizing pneumonia, eosinophilic pneumonia would respond to steroids, underwent bronchoscopy with biopsy due to concern for Pulmonary Alveolar Proteinosis or malignancy. Bronchoscopy with transbronchial biopsy showed atypical mucinous cell proliferation. Lung biopsy via Video Assisted Thoracoscopic Surgery showed mucinous adenocarcinoma (MA) which is an uncommon subtype of lung adenocarcinoma. It responsible for 2.2 3.9% of resected adenocarcinomas [1]. The most frequent symptoms are dyspnea, cough with sputum and fever which are nonspecific and mimic pneumonia. Typical chest CT findings of organizing pneumonia include peripheral, bilateral, wedge-shaped ground glass or consolidative changes (photonegative pulmonary edema) which are very similar to the radiologic presentation of MA which include multicentric opacities or consolidation, ground glass opacities, and nodules, commonly located in the lower lobes [2,3]. Given its slow growing nature, PET-CT avidity would be low, therefore not helpful. According to Liu et al. the yield of surgical lung biopsy and CT-guided percutaneous lung biopsy had a diagnostic yield of 100%, TBLB combined with bronchoalveolar lavage had a diagnostic yield of 80.9% [4] (Figure 1).
Figure 1 H&E slides show lung parenchyma that has been replaced with confluent neoplastic columnar cells with mucinous cytoplasm. Supportive immunostains (not pictured) showed the neoplastic cells are positive for CK7 while being negative for CK20 and CDX2, compatible with a well differentiated mucinous lung adenocarcinoma.
REFERENCES
- Mansuet-Lupo A, Bobbio A, Blons H, Becht E, Ouakrim H, Didelot A, et al. The new histologic classification of lung primary adenocarcinoma subtypes is a reliable prognostic marker and identifies tumors with different mutation status: the experience of a French cohort. Chest. 2014; 146: 633-643.
- Cha YJ, Kim HR, Lee HJ, Cho BC, Shim HS. Clinical course of stage IV invasive mucinous adenocarcinoma of the lung. Lung Cancer. 2016; 102: 82-88.
- Kim TH, Kim SJ, Ryu YH, Chung SY, Seo JS, Kim YJ, et al. Differential CT features of infectious pneumonia versus bronchioloalveolar carcinoma (BAC) mimicking pneumonia. Eur Radiol. 2006; 16: 1763-1768.
- Liu Y, Li J, Wang S, Chen M, Zhao J, Jiang D, et al. Advanced Pneumonic-type Lung Carcinoma: A Retrospective Study of Clinical-radiological-pathological Characteristics with Survival Analysis in A Single Chinese Hospital. Zhongguo Fei Ai Za Zhi. 2019; 22: 329-335.