Costly Condoms or Costly Risks
- 1. Department of Pediatrics and Adolescent Medicine, Albany Medical Center Hospital, USA
Abstract
Male latex condoms (MLCs) serve as prevention and reduce the transmission of sexually transmitted infections (STIs). Limited access and availability, however, can lead to underutilization. To evaluate cost and the current purchase barriers in the commercial setting, I visited 62 national chain pharmacies (NCPs), 76 independent pharmacies (IPs), 58 grocery stores (GSs), and 146 convenience stores (CSs) throughout jurisdictions impacted by STIs. Additionally, since many recipients of governmental health insurance have access to condom coverage, I examined the condom coverage of 25 private health insurance companies (HICs). Overall, it was discovered that NCPs marketed MLCs at the highest cost, while IPs and GSs were similarly priced and marketed MLCs at the lowest price. The average cost of MLCs was lower in high poverty jurisdictions. Also, access to MLCs in various outlets was often impacted by restricted commercial settings. Finally, HICs commonly declared MLCs over-the-counter products. Some also claimed MLCs lack medical importance. For prevention and the benefit of society, an improvement in access to MLCs is in demand.
Keywords
• Male latex condom
• Prevention
• Sexually-transmitted infection
• HIV
Citation
DeMase DF (2017) Costly Condoms or Costly Risks. J Family Med Community Health 4(8): 1137.
ABBREVIATIONS
MLCs: Male Latex Condoms; PrEP: Pre-Exposure Prophylaxis; HIV: Human Immunodeficiency Virus; STI: Sexually-Transmitted Infection; NCP: National Chain Pharmacy; IP: Independent Pharmacy; CS: Convenience Store; GS: Grocery Store; OC: Outlet Category; OTC: Over-the-Counter; BTC: Behind the Counter; NYC: New York City; NYS: New York State; HIC: Health Insurance Company
INTRODUCTION
In New York State (NYS), the human immunodeficiency virus (HIV) has been a challenging epidemic. Current statistics indicate that approximately 123,000 residents within the state are HIV-infected, and nearly 8% of them were unaware of their positive serostatus [1]. An estimated 3,000 new infections appear annually [1,2].
To reduce the number of infections, save lives, provide treatment, and improve the health status of residents, Governor Andrew Cuomo has initiated the Ending the AIDS Epidemic Program. Reducing the annual number of new HIV infections to 750 by the end of the year 2020 is the overall goal [2]. To accomplish this goal, a three-point plan has been devised and accomplishes the following:
- “Identifies persons with HIV who remain undiagnosed and link them to health care [2].”
- “Links and retains persons diagnosed with HIV in health care to maximize viral suppression so they remain healthy and prevent further transmission [2].”
- “Facilitates access to PreExposure Prophylaxis (PrEP) for high-risk persons to keep them HIV-negative [2].”
In addition to PrEP, male latex condoms (MLCs) serve as prevention. Hence, they should allow the governor’s goal to be accomplished. There are, however, a multiplicity of factors that contribute to the underuse of condoms. While blame for nonuse is frequently placed on religion and morality, lifestyles such as sex work and substance abuse are common reasons why condoms fail to be used consistently [3]. Female oral contraceptives and issues ranging from discomfort to a lack of knowledge are responsible for the underutilization of condoms [3-5]. Furthermore, relationship concerns, especially commitment, have served as barriers [3-5].
Social pressures related to economics also explain why several sexually-active persons disregard condoms [3-5]. Poverty-stricken African American men have admitted to cost being a barrier [4,5]. To assist individuals in gaining access more easily, state health departments, Planned Parenthood, medical clinics, and gay and lesbian support centers frequently dispense condoms at no cost. Moreover, Medicaid plans in NYS [6] and other states provide condom coverage, often with a prescription.
Because condoms serve as STI-reducing devices, it is obvious that all sexually-active persons benefit from their use. Furthermore, condoms are the male contraceptive. Thus, coverage by a health insurance company (HIC), governmental or non-governmental, would serve society and be comparable to the Affordable Care Act’s mandatory coverage of female contraceptives. Female contraceptives include not only oral birth control, but also female condoms. Any reason a HIC may refuse to provide condom coverage to males should be identified. To obtain these data, the policies of different HICs were examined.
Finally, after a general observation that variation with condom retail existed throughout different outlets within a neighborhood of Albany, New York, it was postulated that such variations could interfere with condom access and therefore the state’s Ending the AIDS Epidemic Program. In 2010, Rizkalla et al., studied the retail access and availability of MLCs [7]. Due to the time lapse, and in effort to identify current impediments, a similar study was conducted. While the methods for this study had some similarities, including a jurisdiction and the classes of commercial settings visited, the study was broader and included additional high-risk territories as Rizkalla et al., suggested for future studies. The cost of MLCs was incorporated into this study as well, since cost is a known barrier to condom use and to my knowledge, has not been studied in detail. In summary, identifying factors that contribute to the underutilization MLCs was the objective of this study.
METHODS
Sale of Condoms
Participating Entities: National chain pharmacies (NCPs), independent pharmacies (IPs), grocery stores (GSs), and convenience stores (CSs) throughout Albany County of NYS and New York City’s boroughs of Manhattan and the Bronx were visited to study the commercial access of MLCs. These geographic locations were selected, because STIs have significantly impacted the residents over time. The CSs included bodegas, corner stores, delis, and mini marts, some of which were affiliated with gas stations.
Due to the significant social differences between uptown Manhattan and midtown-downtown Manhattan, these jurisdictions were independently analyzed. Uptown Manhattan included all neighborhoods above 59th Street. Midtown-downtown Manhattan included neighborhoods from 59th Street and below.
Measures: To study the commercial access and availability of MLCs, the general sale of the product was assessed. Concurrently, while the average cost of MLCs was studied, the methods by which outlets offered the items were examined as well.
Procedure: With the exception of the IPs of Albany County, each sample was randomly selected through an online search and computer randomization. Due to the scarcity of IPs in business within Albany County, random selection of this outlet category (OC) within this jurisdiction was not an option.
For approximately 10 days, over a time period of four months, MLCs were studied based on OC and geographical location. Prices were documented according to the quantity of MLCs sold within a box, OC, and geographical location. All types and brands of MLCs were included in the sample pools. No restrictions were placed on the number of boxes of MLCs that comprised the sample pools. Some outlets had a wider selection of MLCs than others. Furthermore, the same brands were frequently sold throughout all OCs. Because all condom-selling establishments visited sold boxes with a quantity of three condoms per box, and sometimes single condoms, this study focused on these quantities. The average was calculated according to cost per box within an OC and particular jurisdiction.
Finally, when the MLCs were sold under restricted settings, store clerks and/or managers were asked to provide the prices, as well as the reasons why the MLCs were sold under such conditions. Employees were also approached when MLCs could not be found. In this way, prices could be obtained or the conclusion that MLCs were not sold could be made.
Analysis Plan: Statistical analysis was by analysis of variance (ANOVA) with effects of geographic location, outlet type, and their interaction. Multiple comparisons were by Tukey’s HSD test (Minitab statistical software and Statistica statistical software). The dependent variable was cost per box.
The ANOVA included independent variables for a main effect of geographical location (with four levels: Albany, Bronx, Uptown Manhattan and Midtown-Downtown Manhattan), a main effect of outlet (with 4 levels: national chain pharmacies, independent pharmacies, grocery stores and convenience stores), and their interaction. A significant interaction indicates that the effect of location differs for each outlet type. All effects (location, outlet and their interaction) were statistically significant at the p<0.001 level. The significant interaction indicates that the effect of outlet type on price was different for the four locations.
The average costs were plotted. The overall average cost of a box of MLCs according to outlet category is presented in Figure 1.
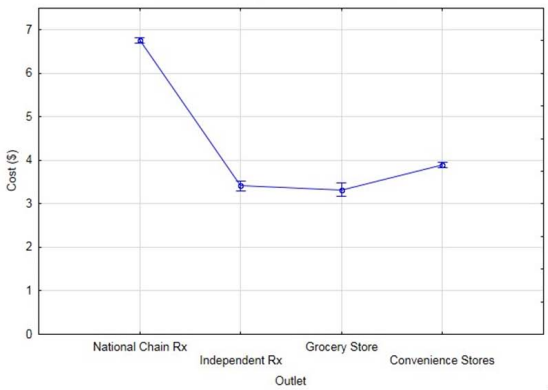
Figure 1 Average cost per box of male latex condoms among different outlets. Error bars indicate 95% confidence interval for the mean.
Figure 2
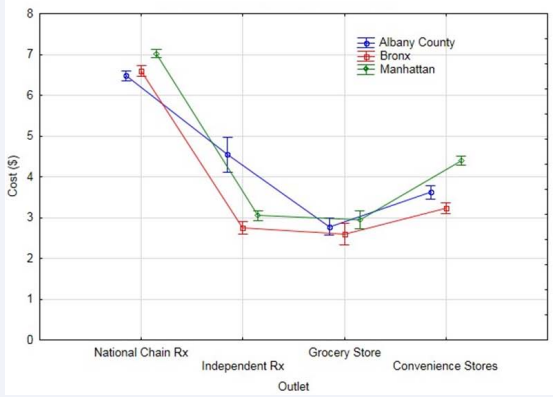
Figure 2 Average cost per box of male latex condoms among different outlets in primary locations. Error bars indicate 95% confidence interval on the mean.
and Figure 3 present average cost according to outlets in particular geographical locations.
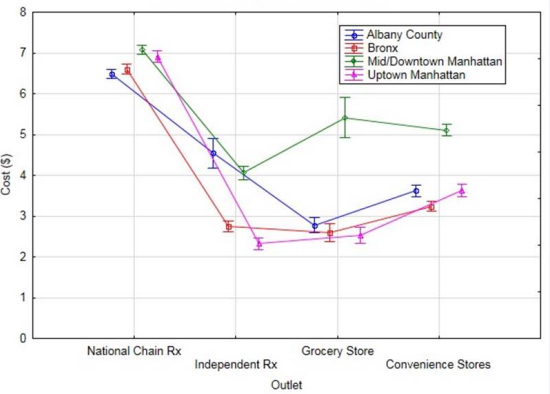
Figure 3 Average cost per box of male latex condoms among different outlets in the four locations sampled. Error bars indicate 95% confidence interval on the mean.
Health Insurance Coverage
Participating Entities: To study non-governmental health insurance condom coverage, 25 HICs throughout California, New York, Texas, Maryland, and Pennsylvania were contacted. These states are among the top ten states that have the greatest number of HIV diagnoses, according to the Center for Disease Control [8]. The identity of the HICs remained confidential.
Measures: To study health insurance coverage of MLCs, the policies and prescription formularies of different non-governmental HICs were examined. Reasons MLCs failed to be covered were investigated.
Procedure: Non-governmental HICs were contacted telephonically after being randomly selected through an online search and computer randomization. Employees, including managers, associated with the company’s Department of Sales, Department of Member Services, and/or Department of Claims and Benefits were questioned about the company’s policy of MLC coverage. Reasons for the lack of coverage were requested.
Analysis Plan: The fraction of non-governmental HICs providing MLC coverage was calculated. When coverage was not offered, reasons were identified and compared.
RESULTS
Cost
Per box of three: Without regard to geographical location, it was evident that NCPs were most costly at marketing MLCs. GSs were noted for marketing boxes of MLCs at the lowest average price.
However, as indicated by the 95% confidence intervals (CIs) in Figure 1, the prices of MLCs at IPs were essentially equivalent to those marketed at GSs. Furthermore, a marginal, yet statistically significant cost difference existed between the average cost of MLCs marketed at CSs and those at IPs and GSs. Figure 1 denotes this general cost pattern. As illustrated in Figure 2 and Figure 3, further analysis of these data present additional trends, particularly the geographical similarities and differences.
Throughout the primary jurisdictions, the general cost pattern was observed. MLCs were consistently most costly at NCPs. GSs frequently marketed the products at the lowest average cost, especially in Albany County and the Bronx. While IPs appeared to sell MLCs at the lowest average cost throughout Manhattan, Table 1 and the 95% CIs in Figure 2 demonstrate that the GSs in this jurisdiction priced MLCs similarly.
Table 1: Condom prices throughout different jurisdictions and outlets.
| Jurisdiction | Outlet | No. outlets visited | Sample size | Average price per box (Avg ± SD) | Price Range |
| Albany County | NCPs | 17 | n=186 | $6.47± 0.52 | $4.99 - $7.39 |
| NYC¹ | NCPs | 45 | n=445 | $6.87± 0.67 | $5.49- $8.99 |
| Bronx | NCPs | 16 | n=160 | $6.60± 0.52 | $5.49- $7.99 |
| Manhattan² | NCPs | 29 | n=285 | $7.02± 0.54 | $5.49- $8.99 |
| Manhattan³ | NCPs | 18 | n=177 | $7.08± 0.69 | $5.49- $8.99 |
| Manhattan4 | NCPs | 11 | n=108 | $6.90± 0.69 | $5.49- $8.29 |
| Albany County | IPs | 6 | n=16 | $4.54± 2.295 | $1.56- $8.43 |
| NYC¹ | IPs | 70 | n=296 | $2.93± 1.196 | $1.29- $7.23 |
| Bronx | IPs | 29 | n=114 | $2.74± 0.987 | $1.49- $5.99 |
| Manhattan² | IPs | 41 | n=182 | $3.05± 1.30 | $1.29- $7.23 |
| Manhattan³ | IPs | 17 | n=76 | $4.06± 1.34 | $1.49- $7.23 |
| Manhattan4 | IPs | 24 | n=106 | $2.32± 0.59 | $1.29- $4.29 |
| Albany County | GSs | 10 | n=64 | 2.78± 0.30 | $1.99- $3.19 |
| NYC¹ | GSs | 48 | n=104 | 2.80± 1.028 | $1.49- $5.99 |
| Bronx | GSs | 20 | n=43 | 2.59± 0.829 | $1.79- $5.99 |
| Manhattan² | GSs | 28 | n=61 | 2.95± 1.1310 | $2.95- $5.99 |
| Manhattan³ | GSs | 10 | n=9 | 5.41± 0.5411 | $5.41- $5.99 |
| Manhattan4 | GSs | 18 | n=52 | 2.53± 0.4612 | $2.53- $3.35 |
| Albany County | CSs | 38 | n=121 | $3.61± 0.67 | $2.69- $5.39 |
| NYC¹ | CSs | 108 | n=362 | $3.90± 1.1013 | $1.58- $7.00 |
| Bronx | CSs | 50 | n=156 | $3.23± 0.6014 | $1.99- $5.00 |
| Manhattan² | CSs | 58 | n=206 | $4.40± 1.15 | $1.58- $7.00 |
| Manhattan³ | CSs | 24 | n=107 | $5.10± 0.85 | $4.00- $7.00 |
| Manhattan4 | CSs | 34 | n=99 | $3.63±0.92 | $1.58-$5.99 |
(Footnotes)
1 Includes the Bronx and Manhattan
2 Includes downtown, midtown, and uptown Manhattan
3 Includes midtown-downtown Manhattan (neighborhoods from 59th Street and below)
4 Includes uptown Manhattan (neighborhoods above 59th Street)
5 This average is based on five of the IPs visited. One pharmacy did not sell condoms.
6 This average is associated with 67 of the IPs visited. Three outlets provided free condoms.
7 This average is associated with 26 of the IPs visited. At three pharmacies, all condoms were free.
8 This average is associated with 34 of the GSs visited. Fourteen outlets visited did not sell condoms.
9 This average is associated with 14 of the GSs visited. Six outlets visited did not sell condoms.
10 This average is associated with 20 of the GSs visited. Eight outlets visited did not sell condoms.
11 This average is associated with six of the GSs visited. Four outlets visited did not sell condoms.
12 This average is associated with 14 of the GSs visited. Four outlets visited did not sell condoms.
13 This average is associated with 105 of the CSs visited. Three outlets visited offered only single condoms.
14 This average is associated with 47 of the CSs visited. Three outlets visited offered only single condoms.
With the exception of IPs, the average cost of MLCs at the OCs appeared to present no vast price differences throughout any of the primary jurisdictions. Overall, however, the Bronx appeared to be the primary jurisdiction that marketed MLCs at the lowest price. As particular regions within Manhattan were explored, cost distinctions continued to be observed more precisely.
As illustrated in Figure 3, the outlets located in the midtown-downtown neighborhoods of Manhattan were more costly than those located in the uptown neighborhoods. The average cost of MLCs marketed in midtown-downtown NCPs was approximately $7.08 per box and higher than those marketed uptown and in Albany County by no more than $0.61 per box (Table 1).
Likewise, the average cost for a box of MLCs sold at the CSs, GSs, and IPs of the midtown-downtown region ranged from $4.06 to $5.41. Hence, these outlets were 29-53% more costly than outlets of the same class located in the uptown jurisdiction, which ranged from $2.32 to $3.63 (Table 1 and Figure 3). In the Bronx, the average cost of MLCs at GSs and IPs was $2.59 and $2.74, respectively, and differed from those available throughout uptown Manhattan by no more than 15% (Table 1 and Figure 3).
As indicated by the ANOVA in Table 2,
Table 2: Analysis of Variance.
| Source | DF | Adj SS | Adj MS | F-value | P-value |
| Geographical location | 3 | 39.85 | 13.283 | 23.34 | 0 |
| Outlet | 3 | 946.83 | 315.611 | 554.61 | 0 |
| Geographical location * Outlet | 9 | 196.07 | 21.786 | 38.28 | 0 |
| Error | 1581 | 899.7 | 0.569 | ||
| Total | 1596 | 5941.04 |
there was a significant effect on outlet type, F (3, 1581) =554.6, p<0.001. The effect on geographical location was also significant, F (3, 1581) =23.34, p<0.001. Furthermore, their interaction was significant, showing there was a difference between outlets in jurisdictions, F (9, 1581) =38.3, p<0.001.
Finally, as noted in Table 1, MLCs were more broadly priced at IPs and CSs. Likewise, the NYC outlets, especially those located in Manhattan, were more broadly priced than those located in Albany County.
Singles: Some of the CSs and IPs visited offered only single condoms, while some offered packaged ones in addition. Overall, it was observed throughout the Bronx that 72% (36/50) of CSs and approximately 17% (5/29) of the IPs visited provided single condoms. In Manhattan, single condoms were unavailable in the midtown-downtown CSs visited. In the uptown neighborhoods, however, approximately 61% (20/34) of CSs and 4% (1/24) of IPs visited offered single condoms. Likewise, 52% (16/31) of the CSs visited in Albany County, especially ones located in the more urbanized neighborhoods, sold single condoms. Neither NCPs nor GSs in any jurisdiction marketed single condoms.
Although single condoms were available at CSs and IPs, the expense at which they could be purchased differed among the two OCs. The majority of CSs throughout all regions routinely marketed single condoms for a price that ranged from $0.50 to $1.25 per condom. Larger-sized condoms were most costly. Concurrently, in NYC, the single condoms available at the IPs and a fraction of the CSs were cost-free and supplied by the Department of Health.
Commercial Access
NCPs throughout Albany County, the Bronx, and Manhattan frequently marketed MLCs from an open display. At most NCPs, the MLCs were placed in close proximity to the pharmacy, as well as in the “Family Planning” aisle. On occasion, however, NCPs in each of the jurisdictions visited did market MLCs in a restricted manner and from locked or simple alarmed settings.
Nearly every CS visited throughout the Bronx and Manhattan offered MLCs from behind the counter (BTC). Approximately 19% (6/31) of the CSs visited in Albany County, however, marketed MLCs from an open display.
The condom-selling IPs of Albany County consistently marketed MLCs from BTC. One IP visited (1/6) failed to sell condoms due to the majority of customers being senior citizens. The selling practices of IPs located in NYC, however, varied. Eighty-one percent (21/26) of all condom-selling IPs visited in the Bronx and approximately 40% (16/41) of those visited in Manhattan offered MLCs in a restricted manner and primarily from BTC. Furthermore, the midtown-downtown neighborhoods of Manhattan were less likely to sell MLCs from BTC than the uptown neighborhoods. While 94% (16/17) of the midtown-downtown IPs visited sold MLCs from an open display and in close proximity to the pharmacy, only 42% (10/24) of the uptown IPs visited marketed MLCs in the same way.
MLCs were marketed in all of the GSs visited in Albany County, primarily in the “Family Planning” aisle. They were not as accessible in the GSs of NYC, however. A significant access barrier pertained to general availability. Approximately 30% (6/20) of the GSs visited in the Bronx and 28% (8/28) of those visited in Manhattan failed to sell MLCs. In addition to theft, managers provided reasons that ranged from “pharmacies being up the street” to the product “never selling when it was available.”
In the GSs that did market MLCs, it was common for the product to be highly secured. At 50% (7/14) of the condom-selling GSs visited in the Bronx, 55% (11/20) of those visited in Manhattan, and 18% (2/11) of the GSs visited in Albany County, MLCs were available from a locked case located in close proximity to the cashiers. Similarly, 50% (7/14) of the condom-selling GSs visited in the Bronx, 45% (9/20) of those visited in Manhattan, and 18% (2/11) of the GSs visited in Albany County marketed MLCs from BTC. One company in Albany County consistently marketed condoms from behind the pharmacy, causing customers to be denied access after pharmacy hours.
Finally, in all jurisdictions, the primary reason given for MLCs being placed in restricted settings was the high theft nature of the product. The high crime rate of some locations also contributed to more secure selling practices.
Insurance and Condom Coverage
Twenty-three of the 25 non-governmental HICs contacted were willing to discuss their policies. All participating companies are similar, inasmuch as none insure MLCs.
The primary reason MLCs are excluded from the plans of coverage is that they are considered over-the-counter (OTC) products. Hence, they are ineligible for prescription. Three HICs in New York first placed blame on employers and did not identify MLCs as OTC products until being questioned about unemployed, financially-secure patients who are capable of purchasing health insurance plans independently.
Furthermore, a HIC in Texas emphasized that no state or federal mandate to cover the cost of MLCs has been enacted. Concurrently, at least one HIC in every state, and overall 26% (6/23) of HICs comprising the sample, claimed MLCs are not “medically necessary.” Upon being asked to define this term, responses included “vital to life,” “a benefit for life,” and “necessary to address medical conditions.” Additionally, in the process of describing “medically necessary,” multiple HICs routinely referred to the glucometer, an instrument used by persons with diabetes to assess glucose levels.
DISCUSSION
Cost
In 2015, 13% of Albany County residents lived below the federal poverty line [9]. Approximately 31% of the Bronx residents and overall, 18% of Manhattan residents, lived similarly [10]. Within these primary jurisdictions, however, different regions experienced different degrees of poverty. While the East Harlem and Washington Heights neighborhoods of uptown Manhattan experienced poverty rates of 31% and 27%, respectively, the Greenwich Village and Soho neighborhoods of downtown Manhattan each had a poverty rate of approximately 8% [10-12]. Based on these recent statistics and the data collected, it is evident that an inversely proportionate relationship often exists between the average costs of MLCs and poverty rate of a jurisdiction. Outlets located in the least poverty- stricken jurisdictions, Albany County and midtown-downtown Manhattan, often market boxes of MLCs at the highest average cost. The average price of MLCs tends to be lowest in the outlets of uptown Manhattan and the Bronx, the poorest jurisdictions of this study (Table 1).
Despite being frequented by the least poverty-stricken, midtown-downtown Manhattan is heavily affected by HIV, chlamydia, and gonorrhea [13]. While uptown Manhattan and the Bronx contrast from midtown-downtown Manhattan with respect to poverty level, they are similar in regards to the infection rate of STIs [13]. The cost of MLCs may contribute.
As illustrated in Figure 3, midtown-downtown Manhattan marketed MLCs at the highest average cost. Because the poverty rates in uptown Manhattan and the Bronx are significantly higher, there is the possibility that some residents in these neighborhoods believe MLCs are unaffordable. Essential living products that fail to be governmentally subsidized may take precedence. Considering substance abuse is notoriously higher in jurisdictions of higher poverty [14], funding an addiction may be of higher priority to some, as admitted to Essien et al., [4]. Hence, it is undoubtful that residents in many jurisdictions hold the perspective that outlets are over-priced.
Price Dispersion
In some jurisdictions, as denoted by the standard deviations calculated and price ranges observed (Table 1), price variation existed among various OCs, or sellers. The variation was more extensive among some sellers and in some locations than in others. From the price variation that appeared, the basic economic principle of price dispersion was evident.
As a result of the price dispersion throughout the different outlets and jurisdictions, it is unlikely that customers are always aware of the locations that market MLCs at the most desirable prices. Frequently, customers are familiar with only one price for products [15]. Some persons may be restricted and have limited access to particular outlets. Others may prefer making purchases only at specific locations. Furthermore, as Burke et al, discovered, some customers prefer certain brands of condoms [16]. The selection of MLCs is broader in some locations than in others, however.
Because the NCPs are highly recognized for health and hygiene products, they may provide some persons with more security than CSs at the time of purchasing MLCs. While some persons may be willing to pay more, some may refuse and place themselves at risk, even when there is shortage of a preferred brand. In consequence to the price dispersion, the social issues remain.
Condom Commercial Accessibility
MLCs are available at the majority of commercial locations. As current data are compared to the observations of Rizkalla et al [7], it is evident that condom availability has improved. Over twice the number GSs within the Bronx currently market MLCs. The fraction of CSs selling MLCs increased as well. The current placement of condoms in the pharmacies and stores is not always ideal and does not always grant customers easy access. The preferred open settings and specific shelving methods which ease condom purchasing, according to Sheldon-Scott et al. [17], are not particularly common. Instead, the highly secure placement observed by Rizkalla et al., in the Bronx remains a common practice. It is also common in multiple Albany County and Manhattan outlets.
Embarrassment likely results and is a purchase barrier [18- 20]. Self image and self presentation are common concerns. Individuals have previously expressed discomfort purchasing condoms as their anonymity decreased and visibility increased [19]. Because many, especially the youth, believe condom use and purchase may be misperceived for casual sex, STIs, and promiscuity [19], they often are deterred from purchasing the products. Having the opportunity to purchase condoms privately and independently is appreciated more than having to rely on the assistance of another party. Also, the restricted setting has led to the belief that condoms are forbidden [17].
Because the prevalence of STIs is higher in regions where these undesirable and restricted retail conditions are more common, it can be argued that the observed conditions are impacting condom purchase, condom use, and therefore the STIs. Until the selling approaches are modified, or cost-free MLCs become available at more locations, the retail conditions will continue to act as a culprit for the public health issues.
Finally, as respondents revealed, condoms are not always available for purchase. Frequently, they are placed out-of-reach, because they are high theft products. Inasmuch as the public is notorious for shoplifting MLCs at a high frequency, it is evident that individuals have a strong desire to use them and engage in risk-free sexual practices. For the benefit of society, selling methods and accessibility should improve.
Insurance Coverage
Condoms are similar to vaccines, for their dual role as STI barriers and a contraceptive classifies them as primary prevention. However, because the non-governmental HICs deny their coverage, it can be questioned if the complete purpose and valor of MLCs are fully understood by the non-governmental HICs.
As MLCs are excluded from plans of coverage, their efficacy and cost-effectiveness are overlooked. Aside from the costs related to unplanned pregnancy, the treatments of STIs are notoriously exorbitant. In 2010, the estimated lifetime cost of HIV treatment was approximately $379,668 per patient [20].
Furthermore, it is common for society to experience an occasional epidemiologic crisis. The international zika virus, for example, recently infected many in the United States. While the mosquito is the primary source of infection, the virus can be sexually-transmitted [21]. Undoubtedly, initial condom coverage has the potential to circumvent infection and costly healthcare services, including those associated with congenital defects. In many ways, despite what some HICs believe, it can be argued that MLCs are vital and do qualify as a medical necessity.
As non-governmental HICs fail to offer condom coverage and individuals engage in unsafe practices, the bioethical principles of beneficence and nonmaleficence are violated [22].
Moreover, a violation of social justice is apparent as Medicaid recipients have access to condom coverage and persons of a higher socioeconomic status receiving non-governmental health insurance do not. Social justice is further violated as females participating in private health plans receive contraceptive coverage, including condoms, and males do not. A simple resolution to these violations would be for all HICs to include condoms in the prescription formularies in the health plans of all patients.
CONCLUSION
From the data collected, it appears that it would be useful for more outlets and public locations to participate in programs that supply and distribute cost-free MLCs to society. While commercial sellers may consider modifying their selling practices, private HICs may consider revising their prescription formularies. Additionally, healthcare providers may contemplate providing routine counseling to all clients. To overcome the challenge of asking, the routine provision of condom prescriptions to the appropriate Medicaid recipients may be effective. The fraction of Medicaid recipients and clinicians aware of the condom coverage by many Medicaid plans, however, warrants questioning. Thus, educating healthcare providers may be essential.
Overall, as access to MLCs improves, the chances that STIs will be experienced less will increase.
ACKNOWLEDGEMENTS
I would like to thank Dr. Paul Feustal, Director of Research at Albany Medical College, for editing the manuscript and assisting with the statistical analysis. I would also like to thank Dr. Michael Gruenthal, Chair of Neurology, for editing the manuscript and reviewing the manuscript prior to submission. Furthermore, I appreciate Dr. Martha Lepow, Professor of Pediatric Infectious Disease; and Dr. Robin Tessinari, Professor of Psychiatry and Internal Medicine, for reviewing the manuscript prior to submission.
REFERENCES
1. New York State Department of Health AIDS Institute (2016) New York State HIV Epidemiologic Profile.
2. New York State Department of Health (2017) Ending the Epidemic 2015-2016 Activity Report.
3. Sakar NN. Barriers to condom use. Eur J Contracept Reprod Health Care. 2008; 13: 114-122.
8. Center for Disease Control (2015) HIV surveillance report.
9. New York State Community Action Association (2015) New York State Poverty Report.
10. New York City Department of Health (2015) New York City Community Health Profiles Atlas.
13. New York City Department of Health. Sexually Transmitted diseases surveillance data.
20. Center for Disease Control and Prevention (2015) HIV Cost Effectiveness.








































































































































