Programa Mais M
- 1. Department of Internal Medicine, Santa Casa de Misericordia de Fortaleza, Brazil
- 2. Centro Universitário Católico de Quixadá, Brazil
- 3. School of Medicine, Universidade Federal do Cariri, Brazil
- 4. Science and Technology Center, Universidade Federal do Cariri, Brazil
Abstract
This study aimed to analyze the initial four years of the Program Mais Médicos (PMM; More Doctors Program) for Brazil, tutored by a public institution from the interior of Ceará from the perspective of the involved actors. Aquanti-qualitative study was proposing with lexical and content analysis using the software IRaMutTeQ version 0.7 alpha 2, R software version 3.4.3, to infer associations between terms used in the speech of the actors involved in the PMM. A statistical association (p-value less than 0.08) was found for 13 of the 130 tests performed. A greater association of words imbued with positive meaning was observed, suggesting the performance of the programis beneficial to the assisted municipalities. On the other hand, the three groups (“assistance”, “supervision”, and “management”) correlated the idea of the program with difficulties, probably faced by the precarious conditions of many municipalities in the interior of the state. The larger context in which the PMM is inserted needs to be re-evaluated alongside the need to better mobilize resources, improve management strategies, produce technologies to facilitate assistance, and customize these to the SUS.
Keywords
• Access
• Primary Health Care
• Public policy
• Phisician supply
• Provision
• Lexical Analysis
• Human Resources
Citation
Júnior JG, de Sales JP, Barros EM, da Silva SBF, Vieira NB, et al. (2020) Programa Mais Médicos: Analysis of the Impressions of the Actors Involved In Brazil. J Family Med Community Health 7(1): 1173.
ABBREVIATIONS
ESF: Family Health Strategy; PMM: Programa Mais Médicos para o Brasil.
INTRODUCTION
In Brazil, despite the important expansion of the EstratégiaSaúde da Família (ESF; Family Health Strategy) in recent years, the capacity for medical training has not kept up with the same speed, nor have sufficient technologies been developed for adequate human resources planning in health [1]. The number of physicians per inhabitant in Brazil in 2015 (2.11 doctors/1000 inhabitants), according to a study on medical demography [2], is small compared to international standards such as France (3.0 physicians/1000 inhabitants), the United Kingdom (2.7 physicians/1000 inhabitants) and Sweden (4.0 physicians/1000 inhabitants) [3], countries which similarly to Brazil have universal/public health systems.
In association with the above, the shortage of professionals with an adequate profile for integral care, coupled with insufficiency and maldistribution, are some of the main barriers to the universalization of access to health, with measures being needed to strengthen competencies and equitable distribution of professionals in these services [4,5].
In this context, the “ProgramaMaisMédicos para oBrasil” (PMM) [6], instituted by Law Nº 12.871, of October 22, 2013, was created. Its main objective is the training of human resources in the medical area for the SistemaÚnico de Saúde(SUS; Unified Health System). In addition, the PMM oversees the provision of doctors in regions where a shortage or absence of these professionals exists, as well as more investments for the construction, reformation and expansion of UnidadesBásicas de Saúde(UBS; Basic Health Units), expansion of the number of medical degree places and medical residency places to qualify the training of these professionals [7,8].
It is noteworthy that the idea of importing labor from other countries is not entirely Brazilian pioneerism. It has already been recommended and used in other countries. French writers such as Doan, Lévy and Pavot [9], argue that one of the ways of balancing emergency medical demands is to attract professionals from other countries to fill vacant posts. In turn, a Canadian study recommends that to minimize the shortage of doctors in this country, as well as measures to reduce migration, a latent reality in Canada, importing doctors would be a possibility [10]. The authors also report that 1 out of 9 physicians interviewed were Canadian working in rural areas of the United States. North American studies have also referred to the importation of medical labor as one of the alternatives to scarcity, especially in rural regions such as Mississippi [11,12].
However, simply providing doctors to demanding areas do not fully address the main problems of accessing health by the part of the population. Ribeiro [13], argues the main problem with primary healthcare is its management and under-financing. The author reports that European countries, Canada, and the United States have a large contingent of foreign physicians serving their population after being certified by a competent national institution. According to that author, the fallacy that medical corporatism in Brazil wants to prevent foreign doctors from being hired is shifting attention from the root of the problem which cannot be solved by hiring more doctors for clinical care, whether they are Brazilian or foreign.
In addition, the literature highlights that there is no nationwide planning ordering the systematic provision of the main resources indispensable for the constitution of a broad Primary Care network, which is powerful enough to alter SUS’s care model and to function as a gateway input has been carried out. In several other countries, such as Spain, Portugal, Canada, and England, a synchronism between the implementation of the national system and the constitution of a Primary Care network occurred, where within a few years, most of these countries managed to secure access to more than 80% of their populations [14].
In this possible divergent scenario, the PMM evaluation works as a feedback tool to assist future decisions regarding the implementation of processes and their achieved results, thus contributing to targeting the necessary interventions [15]. Controversies and differences in opinion exist within the country regarding the adoption of this program as a promotion for the reorientation of basic healthcare and the improvement of healthcare conditions for the most disadvantaged populations. Given it is a recent Program, there have been few studies showcasing the real results already conceived in Brazil, which are inherent to the implementation of this policy [16].
Therefore, this study aims to analyze, through lexical and content analysis techniques, the opinions of medical students, medical supervisors, and municipal managers regarding the impacts (positive and negative), of the four years of PMM operation in a public institution in the interior of Ceará-Brazil, from the perspective of the involved actors.
MATERIALS AND METHODS
Design and participants
A quanti-qualitative study whose sample (not probabilistic, i.e. for convenience) was made up of 40 managers, 212 medical students, and 34 supervising physicians, totaling 289 individuals, working in the 34 municipalities (Appendix I), associated with PMM, under the supervision of a public Higher Education Institution (IES), in the south central region of the state of Ceará, Brazil.
Procedure
Data collection was performed by using form templates at the PMM joint meeting, held in October 2015. Those who attended the meeting and agreed to participate in the study by signing the Informed and Free Consent Term were included in the sample.
The members were divided into three groups: managers, medical students, and medical supervisors. Afterwards, each group was subdivided into eleven arbitrarily chosen subgroups and was ordinally named by the letter “g” with the aim of maintaining anonymity. Each subgroup responded a semi-structured questionnaire (Appendix II), idealized by the authors, containing two questions, one regarding the positive impacts and the other dedicated to the negative impacts of PMM in their respective municipalities.
Data analysis
After tabulation, the data was processed by using the IRaMuTeQ (Interface de R pour les Analyses Multidimensionnelles de Textes et de Questionnaires) software, version 0.7 alpha 2, developed by Pierre Ratinaud, which allows statistical analysis of textual corpus and individual tables/words [17]. IRaMuTeQ provides five types of analysis: classical textual statistics; research regarding group specificities; descending hierarchical rank; similarity analysis and word cloud [18-20].
The answers to each question were transformed into a single Corpus and analyzed through similarity analysis, word cloud, and confirmatory factorial analysis (CFA). The descendent hierarchical classification could not be performed once segment retention was less than 75%, which gives a partial analysis to the findings [18,19].
Before starting the analysis, in the text segment parameters, only “full” language elements were selected as assets: adjectives, unrecognized forms, nouns, verbs; as well as auxiliary nouns and verbs such as complementary (supplementary), with the aim of enriching the text content.
Lastly, from the R software version 3.4.3 [21], Fisher’s Exact Test [22], was used to verify the association between the most frequent terms, presented as follows: Access; Support; Basic Attention; Increase; Length; Difficulty; Lack; Improvement; Health; Link, totaling 130 tests (APPENDIX III).
Ethics approval
This study obeyed the ethical precepts agreed in the Declaration of Helsinki and regulation 510/2016 of the Brazilian National Health Council (CNS), being approved by the Committee in Ethics in Research with Human Subjects under the number 58205216.7.0000.5698.
RESULTS AND DISCUSSION
At the meeting, 30 (75%) managers, 170 (80%) medical students, and 34 (100%) medical tutors attended. For data processing, the corpus consisted of 34 Initial Context Units (ICU) and 81 word segments.
From the graph theory analysis (Figure 1),
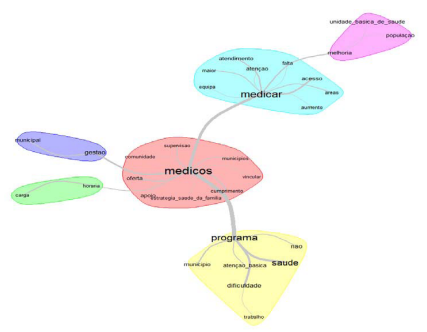
Figure 1 Similarity dendrogram for positive and negative points regarding PMM professionals and students.
occurrences between words can be identified to help understand the structure of the contents from a textual corpus. The figure suggests four main branches from the intrinsic characteristics of the medical practice in the family health strategy (in the centre of the graph), in the following importance order (more solid connecting lines), regarding: (i) the difficulties encountered by the program in complying with actions directed at basic healthcare in municipalities; (ii) specific difficulties with access and service; (iii) the municipal management itself and, finally, (iv) the workload of healthcare professionals in the PMM. It should also be highlighted the natural importance of the PMM in particular and the improvement in basic healthcare units in general, for the adequate care of the population. This information is corroborated by the following comments provided by g10, g12, and g15:
“There is difficulty with the municipality complying with the transfer of aid to doctors. Poor basic healthcare unit infrastructure [...]” (g12)
“There were several difficulties with the implantation of the program in the three municipalities, since they needed to adapt to the routines, spaces, even with the increase in demand for laboratory tests [...]” (g15)
“There was a great improvement in the decrease of professional turnover. Linking professionals with the municipality, increasing integration with management and the community. Compliance with the workload [...]” (g10)
Figure 2 summarises the results from CFA, highlighting three main groups. We chose to call the group in red the “management group”, the blue group the “supervisor group”, and the green group the “assistance group”. The two factors indicated in the analysis, labeling the axes, were named “Attendance to Population” corresponding to factor 1, and “Lack of Medical Professionals” corresponding to factor 2. These two factors were able to capture near 100% of the variability of the frequencies of the terms along the answer of the respondents, indicating the usefulness of the approach.
The “management group” evoked terms such as: population, compliance and care, as well as primary healthcare and the family health strategy in the CFA. In the “supervisory group”, the most evoked words were community, greater, link and support; in the third group, “supervision”, supply, attention and basic healthcare unit were the words with greater evocation force as observed in the factorial plan presented in Figure 2.
These labels represent latent variables, that is, variables that are not directly observable and whose analysis is possible only from variables that reflect their effects [23]. Thus, the latent variable “Attendance to the population” (factor 1), as a linear function of the terms present in Figure 2, suffers a greater positive influence, in this order, from the terms “link” and “community” (from the “supervisory group”), and a greater negative influence from the terms “basic healthcare” and “lack” (“management and assistance groups”, respectively). In fact, positive contributions to the “Attendance to the population” would only be found from the “supervisory group”, while other groups, for the most part, are deficient in this sense, bringing negative contributions, with special lack in the “assistance group”.
On the other hand, in terms of “Medical professionals” (factor 2), the best contributions come from the “offer” and “supervision” (“assistance group”) and the worst from “care” and “municipality” (“management group”). In fact, in general terms, the “management group” does not seem to have played a positive role in terms of both factors, unlike the “supervisory group”. Therefore, it can be inferred positive impacts standing out are from an increase in physician supply and program supervision, although complications associated with the infrastructure and service conditions of the municipality are impasses.
From Table 1, the text segments showing correlation following analysis using Fischer’s exact test, with a 5% significance level, were “workload” with “compliance” and “linking”; “management” with “access”; “health” with “basic care” and “community” with “difficulty”. When the level of significance is raised to 8%, a correlation between the words “medicate” and “access”; “program” and “difficulty”; “supply” with “improvement” and “basic care”; “access” with “improvement”; “community” with “link” and, finally, “increase and support” are observed.
Thus, Table 1 shows the significance levels of the data, from the pairwise association tests, in descending order of dependence. It should be noted that the greatest association occurred between “workload” and “compliance”, highlighting characteristics of the problem. As observed in the following statement:
“We had some very interesting gains such as the professional’s relationship with the municipality, increasing integration with management and community. Compliance with the workload. Financial impact [...]” (g10).
Also in Table 1, the type of association between the mentioned terms can be evaluated based on their odds ratio. The greater/ lower than 1 the odds ratio is, the more positive/negative the relationship between the terms might be, that is, the more a term is quoted/not quoted, the more the other is quoted/no quoted. Hence, the quotation of “workload” leads to the quotation of “compliance”, while the quotation of “management” leads to the non-quotation of “access”, for example. Thus, it may be inferred workload compliance seems adequate, while access involving management suggests greater attention is needed.
From the analysis of Figure 1 and 2, within the three groups: “assistance” (which corresponds to references directly supporting community health); “supervisor” (linked to supervisory activities of fellow physicians); and the “managers” (whose evoked words correlate with health management activities), the words physician, medicate and program stand out in the evoked speeches. This evidence associates medical practice with simple prescription medication and the program as a provider of such demand. This reflects the persistence of the vision of a medical practice based on the hospital-centered model, in which the physician only acts in the prescription of medicines from a curative perspective, contrary to the principles of the SUS and the new National Curricular Guidelines for Medicine Courses [8].
In order to meet the healthcare needs of the population in rural and remote areas, the main objective of the PMM, healthcare professionals should take a biopsychosocial approach to the health and illness process, striving to: i) understand the context of the disease; ii) prioritize care focused on the individual, always stimulating their autonomy; iii) have a close relationship with the community, realizing that it belongs to a wide healthcare network; iv) see each contact with the users as an opportunity for prevention and healthcare education; v) develop skills to deal with typically rural healthcare conditions; vi) stimulate teamwork and vocational training aimed at developing different skills that can assist individuals who, in urban areas, would normally be referred to other places in the healthcare system, in order to reduce obstacles to integral access [24,25].
The association between the word “lack” and the words “basic healthcare unit”, “population” and “improvement” according to the similarity analysis is noteworthy (Figure 1). This may be one of the major impasses for the implementation of the PMM, where the lack of infrastructure of some basic healthcare units or help points that work as such, as well as the lack of input from the municipalities, is evident in speeches. This in turn, may be associated with the words “program”, “difficulty”, “basic healthcare” and “municipality” (Figure 1). In the factorial analysis (Figure 2),
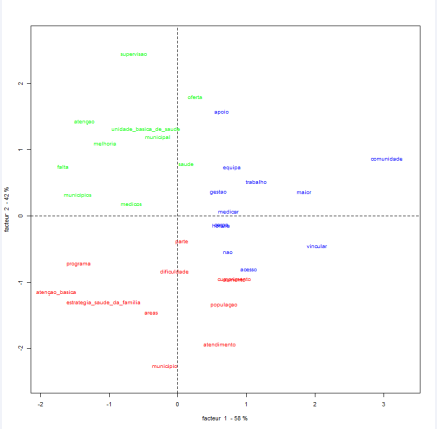
Figure 2 Correspondence factorial analysis regarding PMM professionals and students.
the influence of words such as “support”, “access”, “team” and “community” on Factor 1 (Attendance to the population) is clear, with a statistically significant correlation between “program” and “difficulty” (p = 0.0707) being observed in Table 1. Thus, this description may suggest not the ineffectiveness of the PMM, but reflect the shortcomings and weaknesses faced by local healthcare systems and, therefore, the implementation of the program, as in the following comments:
“One of the major difficulties is compliance by the municipality with respect to the transfer of aid to doctors. Poor basic healthcare unit infrastructure. And help points with minimal service conditions” (g5).
“Lack of previous basic healthcare unit structure for the insertion of the program during the period of program implementation. Increased demand for specialized exams and consultations” (g6).
In fact, looking back at the factor 1 analysis, “Attendance to Population”, the words with the most positive contribution were “offer” and “supervision” (“assistance group”). While for Factor 2, “Lack of Medical Professionals”, a greater negative influence of the terms “basic healthcare” and “lack” (“management and assistance groups”, respectively) were seen. Based on the assumption that both factors are latent variables, that is, they are only seen from variables that reflect their effects, the above statements gain body as they translate difficult operationalization situations of the PMM in some municipalities.
Costa [16], report that basic healthcare faces numerous challenges such as insufficient financing, inadequate UBS infrastructure, low computerization of services and scarce use of the available information for decision making in health management and healthcare, as well as geographical inequalities in the distribution of doctors in the territory.
An essay published in The Lancet reports that in the face of bureaucracy and pre-defined wages in Brazilian laws, as well as with substantial labor costs and the difficulty in firing those who work less, professionals who work in Family Health do not have structured careers, employment or benefits which are granted to other civil servants [26], which increases turnover in FHT and hinders its consolidation in the interior of the country. In addition, Canan, Banggestoss and Moura [14], affirm in their work that high turnover rates in Primary Healthcare suggest dissatisfaction with working conditions.
The correlation between the terms workload and time; municipalities and management suggests one of the great gains of the PMM includes compliance with the workload of professionals in the UBS, facilitating local health management and improving the quality of care for the population (Figure 1).
In Figure 2, factor 2 (“Lack of Medical Professionals”) is negatively associated with words such as basic unit, program, and family health strategy. In table 1,
Table 1: Terms correlated with statistical significance (p<8%) regarding PMM professionals and students.
| Words | p value | Odds ratio | |
| Workload | Compliance | 0.0001 | 34.05 |
| Program | Lack | 0.0122 | † |
| Health | Basic care | 0.0214 | 10.45 |
| Management | Access | 0.0342 | 0.16 |
| Workload | Link | 0.0362 | 6.20 |
| Community | Difficulty | 0.0391 | 0.10 |
| Access | Improvement | 0.0518 | 5.58 |
| Offer | Basic care | 0.0560 | 0.13 |
| Offer | Improvement | 0.0672 | 0.19 |
| Program | Difficulty | 0.0707 | 4.63 |
| Increase | Support | 0.0735 | ?? |
| Community | Link | 0.0737 | 4.92 |
| Medicate | Access | 0.0770 | † |
| † Not calculated due to computational limitations. | |||
the words workload and compliance have statistical significance (p=0.0001), as well as workload and link (p=0.0362), management and access (p=0.0342), and access and improvement (p=0.0518).
These findings suggest an increase in the number of physicians, compliance with professional workload and the population’s access to healthcare, inferring a positive impact on the involved municipalities, as seen in the following comments:
“One of the advantages of the program is the expansion of family health strategy coverage in the municipality. The larger number of people assisted, medical consultations” (g2).
“User satisfaction. Expansion of access in Primary Healthcare. Improvement in the quality of care [...] Increase in the length of stay of medical professional in the Units with a decrease in turnover of professionals” (g6).
“There was a decrease in the turnover of professionals. Linking professionals with the municipality, increasing integration with management and the community” (g10).
A review study published in 2016 [5], underlines that the PMM contributes to the permanence of complete teams in regions with high professional turnover, allowing access and equity in services to historically restricted populations [18,27]. By establishing medical professionals within teams, healthcare in disadvantaged areas expands and contributes to the necessary increase in FHT. The authors also emphasize the PMM coverage is qualified, once professionals fulfill the recommended workload, have adequate training to act in Primary Healthcare and are constantly learning and being educated in the service.
Lastly, the absence of some representatives from each city at the time of data collection and the absence of a questionnaire validated in the literature are limitations of this study.
CONCLUSION
Based on the analysis of the evoked content, a greater correlation of words imbued with positive meaning was observed, suggesting the PMM performance is beneficial to the municipalities assisted in the last five years previously to 2015. The managers did emphasize in their feedback words that imply improvement in increased assistance to the population, compliance with workload by doctors and a decrease in turnover; supervising physicians had their feedback centered more on terms associated with doctor’s support for the community and the prospect of creating a link between them, while physician students focused more on their excerpts in the offer of attention.
In contrast, the three groups correlated the idea of the program with difficulties, probably arising from the precarious conditions of many municipalities in the interior of the state. This indicates a need to rethink the larger context in which the PMM is inserted and the real need to better mobilize resources, optimize management strategies, produce technologies to facilitate assistance and customize it to the SUS, and guide future public policies in healthcare, taking Primary Healthcare as the guiding principle.
Finally, the need to further research this area by listening to the population, stratifying the sample by age, sex, region of the country or basic formation seeking to identify divergences and concurrences within different points of views stands out, which, with that, may contribute to the construction of a healthcare system that is truly universal, equitable and close to local realities.
ACKNOWLEDGEMENTS
We are grateful to the Brazilian Ministry of Education (MEC), Ministry of Health / MaisMédicos Program and School of Medicine, Federal University of Cariri (UFCA).








































































































































