Risk Factors for Ovarian Cancer in a Population of Southeastern Mexico
- 1. Mexican Institute Social Security, Head of Medical Services, México
- 2. Mexican Institute Social Security, Regional General Hospital, México
- 3. Department of General Surgery, Social Security Mexican Institute, México
Abstract
Background: Ovarian cancer is considered the fourth cause of death worldwide according to World Health Organization statistics. Prevention by avoiding risk factors would reduce 30% the incidence of this pathology.
Objective: To describe the ovarian cancer associated risk factors in women of a second level hospital in México.
Material and Methods: Descriptive, transversal study. Forty patient´s with the histopathology diagnosis of ovarian cancer between 2013 and 2016 were included and analyzed. The variables were integrated from files, it be determinate tumor characterizes, clinic evolution, treatment and the factor risk. Were calculated frequencies, and confidence interval 95% (CI 95%).
Results: The more frequent risk factors associated with the studied population were obesity 48% and null parity (25%). The more frequent protector factor was breastfeeding (53%). A secondary analysis it was completed comparing two groups, group 1 with recurrence after treatment and group 2 without recurrence, showing that risk factors between them have no significant differences, including ultrasonography morphologic index and malignancy risk index.
Conclusion: The risk factors associated with an increased relative risk of ovarian cancer are potentially modifiable. Morphologic index and malignancy risk index allow us to predict the malignancy potential in ovarian lesions to be appropriately derived to oncosurgery service.
Keywords
- Ovarian cancer
- Risk factors
- Obesity
- Recurrence
Citation
Jiménez Báez MV, Silva SP, Muñoz MO, Medina Andrade LA, Jurado LS, et al. (2019) Risk Factors for Ovarian Cancer in a Population of Southeastern Mexico. J Family Med Community Health 6(1): 1168.
ABBREVIATIONS
MRI: Malignancy Risk Index; BMI: Body Mass Index
INTRODUCTION
Ovarian cancer is considered one of the main four causes of death worldwide in the woman, this secondary to the delay in diagnosis. The treatment in early stages of the disease has excellent results, and in advanced stages is associated with recurrences in the next 18 months after surgery [1].
Of the total of patients with ovarian cancer 40% is older than 65 years and the highest incidence is between 75 and 79 years-old [2]. The diagnosis frequently is between 50 to 70 years old in average, unfortunately in advanced stages, with a higher percentage of relapse in 60 and 70% of cases, for absence of adequate diagnostic methods [3].
Many national programs of prevention and timely diagnosis of ovarian cancer have been developed to reduce the morbid-mortality. This prevention reduced in 30% the cases of malignancy tumors thought the reduction of risk factors [4-6].
There exist multiple factors associated to ovarian cancer that have been identified, the more frequent and studied are family history of ovarian cancer [7], nulliparity [8-10], infertility [10- 12], use of ovulation stimulant drugs [11], diet rich in saturated fats [13-18], obesity [13-18], another hormone-dependent tumors like breast, colon or endometrium and smoking [19-26].
Screening
Until today there no exist functional screening program for ovarian cancer. The methods for the diagnosis are expensive and do not allow the diagnosis in early stages of the disease [27,28].
The level of CA-125 has their limitations, including that in clinical stages 1 is only high in 50% of the cases [6,27].
Until 47% of ovarian cancer have high Ca 125 levels, 35-65 U/mL but the 75% of serous type ovarian cancer could present normal Ca 125 levels (<35 U/mL) [28].
Through the performance of transvaginal ultrasound many data like ovarian volume, cystic wall characteristics and presence of septa could be identified and allow us to calculate the malignancy risk (sensibility of 89% and specificity of 70%)
(Table 1) a result of 5 points or higher is suggestive of ovarian cancer [6,28].
Table 1: Morphologic index to the ultrasound identification of ovarian cancer
| Morphologic index | |||||
| Variable | 0 | 1 | 2 | 3 | 4 |
| Cystic wall characteristics | Smooth surface (<3 mm of thickness) | Smooth surface (>3 mm of thickness) | Papillary projections (<3 mm of diameter) | Papillary projections (>3 mm of diameter) | Predominantly solid |
| Tumor volume | <10mm | 10-50mm | 51-200 cm | 201-500 cm | >500 cm |
| Septa structure | Without septa | Thin septal (<3 mm of thickness) | Thick septal (3-10 mm of thickness) | Solid area (>10 mm of thickness) | Predominantly solid |
It is estimated that the probability to find a malignant anexial mass in a non-malignant aspect lesion is about 4-6%. The Malignancy Risk Index (MRI) was described by Jacobs et al. [29], in 1990, and this index identifies patients with high risk of ovarian cancer. The MRI II give us a classification based on the ultrasonography characteristics, the menopausal state and the Ca 125 preoperative values, taking as normal a value under 35 U/ml according to the equation MRI II= U (ultrasound) × M (Menopausal state) × Ca 125 (Table 2) [29,30].
Table 2: Malignancy risk index II.
| Parameter | Value | Score | ||
| USG | Multiloculated cyst | Yes | None= 0 A parameter= 1 2 or more parameters= 4 |
More than 200 is suggestive of malignancy |
| No | ||||
| Solid areas | Yes | |||
| No | ||||
| Bilateral | Yes | |||
| No | ||||
| Ascites | Yes | |||
| No | ||||
| Intra-abdominal metastasis | Yes | |||
| No | ||||
| Menopausal state | Pre menopausal state | 1 | ||
| Post menopausal state | 4 | |||
| Ca 125 | U/ml | |||
| Formula | USG x Menopausal state x Ca 125 | |||
| Abbreviations: USG: Ultrasound | ||||
The evidence support that the screening of asymptomatic women for ovarian cancer do not reduce the mortality. Any surgical procedure realized in asymptomatic women without diagnosis of ovarian cancer would be unnecessary [31].
Recurrence and relapse
The patients in advanced stages would have recurrence in the first 2-3 years after initial clinical response to treatment. About 25-60% of ovarian cancer relapses sites include retroperitoneal lymphatic system, upper abdomen and lungs [32].
The patients with local relapse of ovarian cancer show good prognosis in general. The site of relapse is directly related with survival, with poor outcomes in patients with parenchymal relapse in comparison to peritoneum or lymph nodes [33].
To know and identify the risk factors of the studied population allow us to develop a directed prevention to reduce the incidence of ovarian cancer.
MATERIALS AND METHODS
This is a descriptive study, transversal, retrospective, observational, including patients of all ages, with ovarian cancer diagnosis, during their follow up in the General Regional Hospital No. 17 of the Mexican Institute of Social Security in Cancún, Quintana Roo. The patients were in follow up by oncosurgery or oncology between 2013 and 2016. Patients with another synchronic tumor were excluded and with Krukenberg tumor too.
A systematic review in the Hospital files searching by ovarian cancer diagnosis, confirmed by histopathology, was developed. Demographic and clinic pathological variables were registered and analyzed with SPSS 20.00.
The frequencies of variables were described in percentage or proportions according to the variable. The numeric variables were described by central tendency measures and dispersion ones. The student T test were used when the small sample size require it.
RESULTS AND DISCUSSION
Of a total of 88 cases with ovarian cancer registered in the period between 2013 and 2016 in the consultation of oncology and oncosurgery, only 40 files were included, this secondary to incomplete files in 44 cases and 4 cases with a concomitant diagnosis for exclusion.
The 40 patients to be included were divided in 3 groups according to age, with a higher frequency in patients between 45- 64 years-old with 65% and patients in the group older than 65 years with only 15% (Figure 1).

Figure 1 Frequency of ovarian cancer by age.
The Table 3 shows the characteristics according to histological type, the more frequent is the epithelial with a total of 36 patients (90%), stromal and sexual ducts in 2 patients (5%) and germinal cells in 2 patients (5%).
Table 3: More frequent histopathological type.
| N | % | |
| Epithelial: Serous Mucinous Endometrioid Clear cells Undifferentiated carcinoma |
36 23 3 5 2 3 |
90 64 8 14 6 8 |
| Of the stroma and cords Sexual stroma and cords Of granulosa cells |
2 1 1 |
5 50 50 |
| Of germ cells | 2 | 5 |
The more frequent risk factors include obesity (48%) and nulliparity (25%), being less frequent family history of ovarian cancer (3%) and smoking (13%). The more frequent related factor was breastfeeding (53%) (Table 4).
Table 4: Risk factors and protector factors for ovarian cancer.
| Risk factor | N | % |
| Heredofamiliar history of ovarian cancer | 1 | 3 |
| Personal history of endometrial and /or breast cancer Endometrial cancer Breast cancer |
6 5 1 |
15 83 17 |
| Parity Nulliparity 1-3 pregnancies >4 pregnancies |
10 25 5 |
25 62 13 |
| Obesity Grade I Grade II Grade III |
19 9 2 8 |
48 47 11 42 |
| Smoking 10-49 years >50 years |
5 3 2 |
13 60 40 |
| Early menarche | 6 | 15 |
| Late menopause | 7 | 18 |
| Protector factor | ||
| Breastfeeding 6 months- 1 year >1 year |
21 7 14 |
53 33 67 |
| Use of oral contraceptives 1-3 years >3 years |
4 3 1 |
10 75 25 |
The more frequent clinical stage at the moment of diagnosis was the stage III with 21 patients and the IV stage with 2 patients (Figure 2).
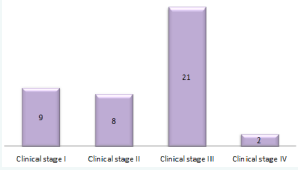
Figure 2 More frequent clinical stages at the moment of diagnosis.
The time between first medical contact and the surgical diagnostic-therapeutic procedure was about three months; in 8 patients the histopathology diagnosis was already established in a private hospital and came to the first consultation to accomplish the adjuvant and citoreduction treatment (Figure 3).
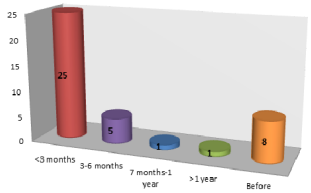
Figure 3 Time between first consultation and surgical procedure.
In none of the cases analyzed was the morphological index or the MRI. Taking the data from the files, the researchers found that in 26 patients (65%) the morphological index could be obtained, of these 20 had a suggestive result to malignancy (77%); the MRI was positive in 100% of cases with a value greater than 200 (Figure 4 and 5).
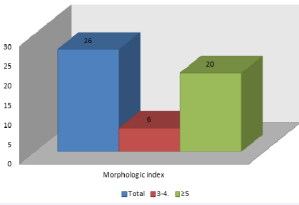
Figure 4 Patients with morphologic index equal or higher than 5.
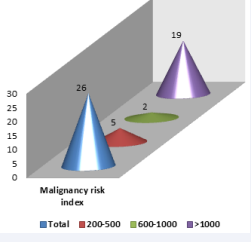
Figure 5 Patients with malignancy risk above 200.
The surgical treatment consists in the surgical tumor removal plus chemotherapy, adjuvant or neoadjuvant; and only one case was treated with adjuvant radiotherapy. The more frequent surgical treatment was the ovarian routine (37%) and less frequent optimal citoreduction with one patient (3%). In total 9 of 40 patients need an interval laparotomy (Table 5).
Table 5: Surgical procedure.
| Surgical procedure | N | % |
| Ovarian routine | 15 | 38 |
| Optimum cytoreduction | 1 | 3 |
| Suboptimal cytoreduction | 10 | 25 |
| Laparotomy + biopsy | 14 | 25 |
| Interval laparotomy | 9 | 23 |
A comparative analysis was performed between patients with recurrence (group 1) and patients without recurrence (group 2), Table 6 shows the results of this analysis. After the analysis it was observed that there were no significant differences between the two groups, except in the smoking variable, in which it was observed that patients with recurrence had longer smoking compared to patients who did not have recurrence.
Table 6: Results from the different variables in group 1 and 2.
| Variable | Group 1 | Group 2 | S.D. |
| Age | 59 years | 52 years | ±11 |
| Smoking | 57 years | 26 years | ±16 |
| Pregnancies | 1.4 | 2 | ±1.7 – 2.91 |
| BMI | 30 | 28 | ±7.3 |
| Menarche | 13 years | 12.7 years | ±2.06 – 7.5 |
| Menopause | 46 years | 46 years | ±7.3 – 4.4 |
| Personal history of breast or endometrial cancer | 2 patients | 0 patients | ±0.42 |
| Abbreviations: BMI Body Mass Index |
The clinical stage according to the group can be seen in Figure (6).
Figure 6 Clinical stages in the group 1 and 2.
None of the ultrasonography parameters of the morphologic index (Table 7) or MRI (Figure 7) were significant to consider them predictive for relapse.
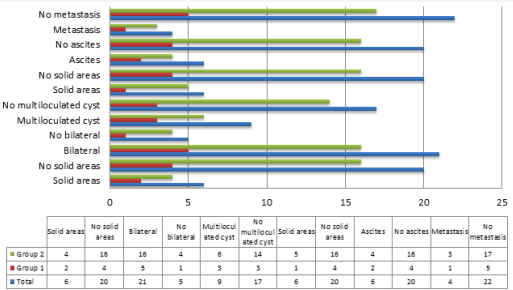
Figure 7 Ultrasonographic parameters and malignancy risk index.
Table 7: Morphologic index.
| Variable | Group 1 | Group 2 | Total |
| Cystic wall characteristics Smooth surface (<3 mm of thickness) Smooth surface (>3 mm of thickness) Papillary projections Predominantly solid |
4 9 2 6 |
1 3 0 1 |
5 12 2 7 |
| Tumor volume 50-200 cm3 200-500 cm3 >500 cm3 |
1 1 3 |
2 4 15 |
3 5 18 |
| Septa structure Without septa Thin septal (<3 mm of thickness) Thick septal (3-10 mm of thickness) Solid area (>10 mm of thickness) |
2 1 2 0 |
12 3 3 3 |
14 4 5 3 |
This was a descriptive, transversal, retrospective and observational study that included 40 patients with diagnosis of ovarian cancer. The age at the moment of diagnosis of those patients was between 45 to 64 years (65%) with a mean of 54.5 years (limits of 27-80 years) and a mode of 49 years, with similar results as the Rivas-Corchado LM et al. [2], study with a mean of 52 years.
The ovarian cancer of epithelial type was presented in 90% of the patients, with the subtypes serous (64%), mucinous (8%), endometrioid (14%), of clear cells (6%) and undifferentiated (8%) completed the frequencies. Jervis S et al. [7], in his study about the histologic subtypes more frequent finds reported the high grade serous and endometrioid.
The obesity (48%) and nulliparity (25%) were the risk factors associated with the studied population. Obesity grade I and III were the more frequent. In a cohort study performed by Barb D et al. [16], it was concluded that obesity is a modifiable risk factor. The average Body Mass Index (BMI) was 29 kg/m2 (20-46Kg/ m2 ), with a mean weight of 65 kg., mode of 45 kg (45-109 Kg), average height of 1.5m (1.3 to 1.69 m). The average parity was 0 with a mode of 2. Stewart LM et al. [8], in a cohort study, conclude that null parity increase three times the risk for ovarian cancer.
Only one case has family background of ovarian cancer, and 6 more have personal background of breast or endometrial cancer. Soliman PT et al. [23], concludes that women with synchronic ovarian and endometrial cancer were young, obese, nulliparous and pre-menopauses’ patients. Metcalfe KA et al. [21], suggests that prophylactic oophorectomy in patients with breast cancer and BRAC1 and 2 mutations for the high association with a metachronic ovarian cancer (12.7% in BRCA 1 and 6.8% in BRCA 2).
In 5 cases it was associated with smoking, with an average age of 35 years-old. In the study Cancer Causes Control, smoking increases the risk of ovarian cancer, especially mucinous subtype [26]. None of the patients had been using ovulatory drugs. The median age of menarche was 12.1 years (10-18 years) and for menopause 44 years with a mode of 47 years (30-35 years). The breastfeeding’s (53%) and use of combined oral hormones (10%) were the more frequent protective factors.
From the 40 patients included 21 were in clinical stage III, only in 9 cases was possible the detection in clinical stage I. According to the third consensus in ovarian cancer 2011, 75% of cases were diagnosed in clinical stage III and IV [6].
In none of the studied cases a screening was realized before, a no predictive scales for malignancy detection were requested, like the MRI or the morphologic index. Once this test were realized by researchers, in the cases were it was possible to integrate the data, the morphologic index was higher than 5 in 77% of the cases. In the other hand the RMI was positive in 100% of cases with values higher than 200.
Reade C et al. [31], performed a meta-analysis concluding that the screening for asymptomatic women for ovarian cancer did not reduce the mortality or the diagnosis in advanced stages and is associated with unnecessary surgical intervention. The performance of MRI is an efficient method to classify post menopause women with adnexal tumors, benign or malignant, with an accuracy of 81.8% according to Trevino-Baez JD et al. [29].
CONCLUSION
Cancer still being a disease with bad prognosis when is detected in advanced stages- Actually there no exist a screening method for early detection. The prevention programs could reduce in a 30% the cases with malignant tumors by a reduction in modifiable risk factors.
Although the sample size it could be observed that the risk factors with higher relative risk for ovarian cancer are predominantly modifiable, including obesity, diet, parity and smoking.
There exist low promotion to encourage protective factors like salpingoclasia or salpingectomy, use of oral hormones, use of aspirin, breastfeeding, low fat meals and vegetables consumption.
In none of the cases morphologic index or MRI were applied. Those scales in patients with adnexal tumors allow us to predict malignancy in ovarian tumors to be referred timely to an oncosurgery service for the appropriate treatment.








































































































































