The Relationships between Insomnia & Depression
- 1. Department of Family Medicine, Kowloon West Cluster, Hong Kong Hospital Authority, Hong Kong
Abstract
Insomnia is a common symptom of depression. In clinical practice, the relationships between insomnia and depression are actually more complex. A literature review was undertaken to find out various possible relationships between insomnia and depression. Research evidences showed that insomnia can be a symptom of depression; insomnia can also be a risk factor of depression; and insomnia can exacerbate/perpetuate depression. Moreover, residual insomnia after treatment for depression is common; and depression may not hinder insomnia outcome. Furthermore, sometimes insomnia and depression do not co-occur. There are also evidences that for patients with both insomnia and depression, insomnia therapy concomitant with depression therapy (e.g. using antidepressant for treating depression plus using cognitive behavioural therapy for treating insomnia) can result in positive treatment outcome in depression. As a result, combination treatment of insomnia and depression may be the future treatment direction for bringing greatest treatment benefits to patients suffering from both depression and insomnia.
Keywords
- Insomnia
- Depression
Citation
Ng CL (2015) The Relationships between Insomnia & Depression. J Family Med Community Health 2(1): 1027.
INTRODUCTION
Insomnia was commonly viewed as a symptom of depression for many years [1,2]. In the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) of the American Psychiatric Association, insomnia is one of the symptoms in the diagnostic criteria of major depressive disorder (MDD) [3]. However, during the last decade, many studies brought evidences that insomnia could be more than a symptom of depression. For example, some studies had found that insomnia pre-exist before onset of depression. Some studies also suggested that insomnia can perpetuate or exacerbate depression. This article will discuss the possible relationships between insomnia and depression, with reference to evidences in scientific research. Based on the possible relationships between insomnia and depression, this article will also propose one treatment approach which is beneficial for individuals who have both insomnia and depression.
DOES DEPRESSION CAUSE INSOMNIA?
Is depression a causative factor for insomnia? A true experimental study is not possible: it is unethical to randomly assign healthy subjects to have depression induced or not, and then measure insomnia. In the philosophy of clinical science, to establish that depression is causing insomnia, two conditions must be fulfilled: (1) Depression must precede insomnia, and (2) Variations in depression and insomnia must covary [4]. The best ways to prove these are quasi-experiments (i.e. observational epidemiology) and randomized clinical trials in treating depression and seeing if insomnia decreases.
Very few studies investigated whether insomnia could follow depression and therefore could be related to depression. This is due to the historical assumption that insomnia is a depressive symptom as opposed to a disorder per se. A large retrospective study (n=14,915) in 4 European countries found that insomnia symptoms appeared before onset of symptoms of first episode of mood disorder (depressive disorders or bipolar disorder) in 41.7% of cases; they appeared at the same time in 29.4% of cases; and insomnia symptoms appeared after the onset of depressive episode in 28.9% of subjects [5]. This showed that although insomnia did appear at same time or after onset of symptoms of depression in 58.3% of cases, insomnia actually appeared before onset of symptoms of depression in 41.7% of cases. This study showed that in individuals with both depression and insomnia, insomnia is not always a symptom of depression.
INSOMNIA CAN BE A RISK FACTOR FOR DEPRESSION
In a longitudinal mental health epidemiologic study, 7954 respondents were questioned at baseline and 1 year later about sleep complaints and psychiatric symptoms. The risk of developing new major depression was much higher in those who had insomnia at both interviews compared with those without insomnia (odds ratio OR, 39.8; 95% confidence interval CI, 19.8 to 80.0). The risk of developing new major depression was much less for those who had insomnia that had resolved by the second visit (OR, 1.6; 95%CI, 0.5 to 5.3) [6].
The Johns Hopkins Precursors Study, a long-term prospective study involving 1,053 medical students with median follow-up of 34 years, was carried out to study the relation between self-reported sleep disturbances and subsequent clinical depression and psychiatric distress. This study showed that for those who reported insomnia in medical school, the relative risk of development of clinical depression was 2.0 (95% CI, 1.2-3.3) [7].
The Zurich Study was a prospective epidemiological study of depressive, neurotic, and psychosomatic syndromes of a sample of 4547 subjects in Zurich. A community sample of 591 young adults within the Zurich Study was selected, and their psychiatric, physical and sleep symptoms were assessed in 6 interviews conducted in the years 1979, 1981, 1986, 1988, 1993 and 1999. Results showed that 17% to 50% of subjects with insomnia lasting 2 weeks or longer developed a major depressive episode in a later interview [8].
These large studies provided evidences that insomnia can be a risk factor for onset of depression.
THE BIDIRECTIONAL RELATIONSHIP OF DEPRESSION AND INSOMNIA
The Nord-Trøndelag Health Study (HUNT) is a large Norwegian population-based prospective study to investigate the relationship between depression and insomnia. 24,715 participants had completed the questionnaires in both HUNT2 (1995-1997) and HUNT3 (2006-2008). Participants who did not have depression in HUNT2 but who had insomnia in both HUNT2 and HUNT3 had an odds ratio (OR) of 6.2 of developing depression in HUNT3. Similarly, participants who did not have insomnia in HUNT2 but who had depression in HUNT2 and HUNT3 had an OR of 6.7 of developing insomnia at HUNT3 [9]. The result of this study supports a bidirectional relationship between depression and insomnia (the causal link works in both directions).
INSOMNIA CAN PERPETUATE/ EXACERBATE DEPRESSION, AND CAN INCREASE RISK OF RECURRENCE OF DEPRESSION
In a multisite RCT involving 1,801 elderly patients with MDD and/or dysthymia, patients were assigned to an insomnia-status group (persistent, intermediate, or no insomnia) based on insomnia scores at both baseline and 3-month time points. Patients were randomized to the intervention arm (management by depression clinical specialist) or usual care arm. Those with persistent insomnia were 3.5 times (95%CI, 1.7-6.9) more likely to remain depressed at 12 months, compared with patients with no insomnia [10].
In another RCT, 60 patients (mean age 41.5 ±12.5 years) with MDD and insomnia received open-label fluoxetine for 9 weeks and also randomized to receive either: (1) blinded eszopiclone 3mg [for treating insomnia] or (2) placebo after the first week of fluoxetine. Results showed that higher level of insomnia (higher Insomnia Severity Index) corresponded to significantly greater intensity of suicidal thinking (higher Scale for Suicide Ideation) (p<0.01) [11].
Furthermore, in a RCT, 116 patients with unipolar depression aged ≥70 who had remitted and remained stable were randomized to 2 years maintenance with: (1) pharmacotherapy; (2) placebo; (3) interpersonal psychotherapy (IPT) + pharmacotherapy; or (4) IPT + placebo. Results showed that residual sleep disturbance (measured by Pittsburgh Sleep Quality Index) was an independent predictor of early recurrence of depression (hazard ratio 1.11, 95%CI 1.03-1.20, p=0.01) [12].
These studies provided evidences that insomnia is a disorder that can maintain depression – by exacerbating/ perpetuating depression, and also by increasing risk of recurrence of depression.
RESIDUAL INSOMNIA AFTER TREATMENT FOR DEPRESSION IS COMMON
In a study, 215 outpatients with MDD were treated openly with fluoxetine for 8 weeks. Of the 108 full responders (Hamilton Rating Scale for Depression score ≤7), only 19 (17.6%) had no residual symptoms of MDD. The most frequent residual symptom in depression was insomnia (44%) [13], the drawback of this study was the lack of a control group.
In another study, the sleep of 30 elderly patients with recurrent unipolar depression was examined at baseline (before treatment) and again in a state of remission with nortriptyline. Perceived sleep quality improved significantly during early continuation therapy with nortriptyline, but not to the level reported by a group of 30 age- and sex- matched healthy controls [14].
These studies showed that residual insomnia after treatment for depression is common.
DEPRESSION MAY NOT HINDER INSOMNIA OUTCOME
In a pre- to post-treatment case series (n=301) conducted by Manber et al (2011) [15], patients in both high depression group (HiDep) (Beck Depression Inventory BDI score ≥14) and low depression group (LowDep) (BDI score <14) received seven sessions of group cognitive-behavioural therapy for insomnia (CBT-I) without direct treatment on depression. Results showed that there was same improvement of insomnia severity in both HiDep and LowDep group (p=0.61). This study showed that depression may not hinder insomnia outcome.
INSOMNIA THERAPY CAN IMPROVE DEPRESSION OUTCOME
A RCT conducted by Fava et al (2006) [16] had involved 545 patients with both MDD and insomnia. This study found that the combination of fluoxetine (antidepressant) and eszopiclone (“Z-Drug” hypnotic) produced higher rate of remission of depression compared with combination of fluoxetine and placebo (42% vs. 33%; p=0.03) at Week 8. The fluoxetine+eszopiclone group also had significantly decreased sleep latency, wake after sleep onset (WASO), increased total sleep time (TST) and sleep quality (all p<0.05).
In another RCT conducted by Manber et al (2008) [17], 30 patients with MDD and insomnia were randomized into: [1] escitalopram (antidepressant) plus 7 individual therapy sessions of cognitive-behavioural therapy for insomnia (CBT-I); or [2] escitalopram plus quasi-desensitization (CTRL, i.e. placebo CBT-I). Escitalopram + CBT-I [i.e. combination therapy of depression and insomnia] resulted in a higher rate of remission of depression (61.5%) than escitalopram + CTRL (33.3%). Escitalopram + CBT-I was also associated with a greater remission from insomnia (50.0%) than escitalopram + CTRL (7.7%).
In a more recent RCT published in 2011, 37 Japanese patients with residual depression (partially remitted mild or moderate depression despite on maximum dose of antidepressant) and refractory insomnia were randomly assigned to either: (1) treatment-as-usual (maximum dose of antidepressant with regular follow-up by psychiatrist); or (2) treatment-as-usual plus 4 sessions of weekly 1-hour brief behavioural therapy for insomnia. At 8 weeks, the combination treatment produced higher rates of remission than treatment-as-usual alone, both in terms of depression (50% vs. 6%) and in terms of insomnia (50% vs. 0%). The combination treatment also resulted in significantly lower GRID-Hamilton Depression Rating Scale (p = 0.013) and lower Insomnia Severity Index (P < 0.0005) at 8 weeks [18].
These studies provided evidence that for patients with both insomnia and depression, the addition of insomnia therapy to depression therapy (i.e. combination treatment of both conditions) can result in positive depression outcomes.
INSOMNIA AND DEPRESSION DO NOT NECESSARILY CO-OCCUR
In some cases, insomnia and depression are unrelated. Among all individuals with depression, the presence of insomnia was found in nearly 75-80% of the subjects [2,19] – meaning that about 20-25% of patients with depression do not have insomnia. On the other hand, according to the Zurich study mentioned above, 17-50% of subjects with insomnia lasting for ≥2 weeks developed a MDD later [8] – this implies that 50-83% of subjects with insomnia did not develop depression. These were evidences that insomnia and depression do not necessarily co-occur.
THE POSSIBLE RELATIONSHIPS BETWEEN INSOMNIA AND DEPRESSION, AND THE IMPLICATIONS
It is obvious that the relationship between insomnia and depression is complex. Based on our literature search, the various possible relationships between insomnia and depression are listed in (Table 1).
Table 1: Possible relationships between insomnia and depression.
| Possible relationship between insomnia and depression | Scientific researches quoted in this article |
| Insomnia can be a symptom of depression | Ref. 5 |
| Insomnia can be a risk factor of depression | Ref. 6,7,8 |
| Insomnia and depression has bidirectional relationship | Ref. 9 |
| Insomnia can exacerbate/ perpetuate depression and increase risk of recurrence of depression | Ref. 10,11,12 |
| Residual insomnia after treatment for depression is common | Ref. 13,14 |
| Depression may not hinder insomnia out com | Ref. 15 |
| Insomnia therapy can improve depression | Ref. 16,17,18 |
| Insomnia and depression do not necessarily co-occur | Ref. 2,8,19 |
Results of scientific research showed that: sometimes depression precedes insomnia; sometimes insomnia comes before depression; sometimes insomnia can also perpetuate/ exacerbate depression. Moreover, residual insomnia after treatment for depression is common; and depression may not hinder insomnia outcome. Furthermore, sometimes insomnia and depression do not co-occur. Thus insomnia and depression do not follow a typical cause-and-effect relationship; and their exact relationship is not always clear. For these reasons, the DSM-5 stated that it is preferable to regard insomnia and depression as comorbid conditions [3].
For a patient having both insomnia and depression, it is usually not easy to find out whether his insomnia had occurred before the onset of depression (primary insomnia), or the insomnia is the effect of depression (secondary insomnia). Thus the DSM-5 has also replaced primary insomnia with the diagnosis of insomnia disorder, a switch to avoid the primary/secondary designation when insomnia co-occurs with other mental disorder (or medical condition) [3].
Among the various research findings on the relationships between insomnia and depression, one finding is actually most impactful: in patients with depression and comorbid insomnia, combination therapy of insomnia and depression can improve depression outcome. This shed new light on the treatment direction of this group of patients.
IMPLICATIONS IN TREATMENT FOR PATIENT WITH BOTH INSOMNIA AND DEPRESSION
According to the Practice Parameters for the Psychological and Behavioural Treatment of Insomnia published by the American Academy of Sleep Medicine, cognitive-behavioural therapy for insomnia (CBT-I) is effective and recommended in the treatment of primary and secondary insomnia [Highest level of recommendation] [20]. For treatment of insomnia, CBI-I has been shown to have similar and more durable benefit than hypnotics [21,22] , and is free of the side-effects of hypnotics.
Based on the guideline of the American Psychiatric Association, psychotherapy is the first line treatment to mild depression, whereas pharmacotherapy is indicated for treating moderate to severe depression [23]. Tricyclic antidepressants (TCAs) are known as sedating antidepressants. Reduced sleep latency, reduced wakefulness during sleep and increased sleep efficiency have been found in the polysomnography in depressed patients treated with amitriptyline [24,25] , doxepin [26] and trimipramine [27]. On the other hand, most of the selective serotonin reuptake inhibitors (SSRIs) and serotonin-norepinephrine reuptake inhibitors (SNRIs) are non-sedating antidepressants (with the exception of fluvoxamine which is highly sedating). SSRI and SNRIs are most widely used antidepressants because of their safety and improved side-effect profiles in comparison to TCAs. However, they can cause significant sleep disruption and worsen insomnia in some patients [28].
According to the evidence-based guideline published in the Journal of Clinical Sleep Medicine (JCSM) in 2008, combination therapy is recommended for insomnia with comorbid conditions (e.g. CBT-I for insomnia plus antidepressant for depression); and sedating antidepressant is recommended for treating insomnia with comorbid depression [29]. This guideline has good agreement with current research evidence that combination therapy for both depression and insomnia will offer best treatment benefit for patients suffering from depression with comorbid insomnia.
As mentioned above, there are evidences that treatment of insomnia in patients having depression with comorbid insomnia can result in positive outcomes in both insomnia and depression. By applying these evidences, and by integrating with the above guidelines, a new treatment approach for patients having both depression and insomnia can be proposed (Figure 1).
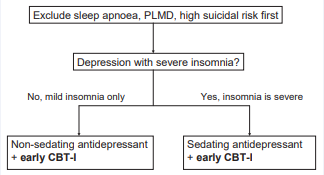
Figure 1 A proposed new treatment approach for an individual having both insomnia and depression. This is based on research evidence that treatment of insomnia in patients with both insomnia and depression can result in positive depression outcome. Abbreviations: PLMD: Periodic Limb Movement Disorder; CBT-I : Cognitive Behavioural Therapy for Insomnia
The principles of this new treatment approach are: (1) The first step in the management of patients with both insomnia and depression is to rule out any other sleep disorders such as sleep apnoea and periodic limb movement disorder (PLMD) [2], and to assess suicidal risk. Urgent referral to psychiatrist is mandatory if patient has high suicidal risk (2) Starting sedating antidepressant with early CBT-I if patient’s insomnia is significant. (3) Starting non-sedating antidepressant with early CBT-I if patient’s insomnia is mild. (Non-sedating antidepressant is the first-line treatment for depression with mild insomnia because of its more favourable side-effects and safety profiles over sedating antidepressants). This is a treatment approach which is beneficial for patients with both insomnia and comorbid depression (by starting early combination therapy).
CONCLUSION
From the evidence of scientific researches, it is obvious that the relationship between insomnia and depression is complex. There are many possible relationships between them: -- insomnia can be a symptom of depression (insomnia emerges at same time or after onset of depression); insomnia can be a risk factor of depression; insomnia can exacerbate/ perpetuate depression and increase risk of recurrence of depression; residual insomnia after treatment for depression is common; depression may not hinder insomnia outcome; sometimes insomnia and depression do not co-occur; furthermore, combination treatment of insomnia and depression can result in positive depression outcomes. In summary, insomnia and depression are co-morbidities and have bidirectional relationship. The finding that has the largest impact is that -- in patients with depression and comorbid insomnia, the addition of insomnia therapy to depression therapy (i.e. combination therapy) can improve depression outcome.
As a result, there are some professional and clinical implications. Firstly, all health care professionals who are involving in treating insomnia and depression (e.g. family physicians, psychiatrists, psychologists) need to aware of the possible relationships of insomnia and depression, so as to deliver more comprehensive medical care to their patients. Secondly, because of the strong association between insomnia and depression, all patients with insomnia should be screened for depression, and vice-versa. Furthermore, concomitant and aggressive treatment of insomnia, in addition to the treatment of depression, may become a future treatment direction for improving morbidity and quality of life of our patients with both insomnia and depression.








































































































































