Uncommon Common Back Pain: A Case of Cervical Myelopathy
- 1. Department of Family Medicine, Loma Linda University Health, USA
Abstract
Ossification of the posterior longitudinal ligament (OPLL), is a progressive disease that typically presents with mild, non-specific symptoms. Symptoms may include neck and low back pain, tingling, and numbness in the upper extremities, and as the disease advances, it may impair activities of daily living. Occasionally, OPLL can be misdiagnosed if imaging is analyzed without considering clinical findings. Therefore, the imaging results need to be correlated with a comprehensive history for diagnostic accuracy. In addition, an evaluation by a spinal specialist should be considered for persistent symptoms to further correlation between imaging and clinical presentation.
Keywords
• Ossification of the posterior longitudinal ligament
• OPLL
• Cervical myelopathy
• Backpain
Citaion
NGUYEN V, IKE B, JAQUA E, SIMON L (2022) Uncommon Common Back Pain: A Case of Cervical Myelopathy. J Family Med Community Health 9(1): 1188.
INTRODUCTION
With approximately 10 to 20 percent of patients presenting for evaluation of neck pain annually, identifying the etiology is of utmost importance to direct the correct treatment plan [1,2]. Myelopathy is a general term used for a neurologic deficit related to spinal cord injury, whereas radiculopathy describes specific nerve root impairment [3]. Patients with myelopathy tend to have a more insidious onset of symptoms that are widespread and variable in distribution. Symptoms can range from tingling and numbness to weakness and spasticity. Myelopathy can also be associated with gait disturbances, decreased hand dexterity, and changes in bowel or bladder function [1].
Degenerative cervical myelopathy (DCM), is an umbrella term that includes cervical spondylotic myelopathy, ossification of the ligamentum flavum (OLF), degenerative disc disease (DDD), and ossification of the posterior longitudinal ligament (OPLL) [2]. Although 22 percent of neck pain is due to DDD, the other causes of DCM are not uncommon [4]. For example, OLF and OPLL affect approximately 4 and 3 percent of the population, respectively [5,6].
Specifically, ossification of the posterior longitudinal ligament (OPLL), can lead to irreversible, devastating spinal cord injury. However, since surgical intervention is the mainstay of treatment, an accurate and prompt diagnosis of OPLL can lead to more timely management, halting further damage to the spinal cord and improving overall morbidity and mortality.
CASE REPORT
A 61-year-old female with a history of asthma, hypertension, and rheumatoid arthritis (RA), presents to her primary care physician with a 6-month history of intermittent tingling in her bilateral hands and feet. The tingling feels like “a bug running and biting [her] fingers and toes.” There is no associated weakness or other neurological findings. The patient was advised to start a vitamin B complex supplement and obtain laboratory evaluations. Complete blood count, metabolic panel, thyroid function, and vitamins B12, ferritin, and D were tested and unremarkable.
The patient had a follow-up evaluation two months after starting a vitamin B complex supplement. Unfortunately, she denies any improvement of symptoms with vitamin supplementation. She continues to have intermittent tingling in her fingers and toes but now reports that tingling is sometimes up to her forearms and lower extremities. She has also developed right leg pain, characterized as a “cramp” on the medial aspect of her distal femur and her knee. Once again, the physical exam is unremarkable, with no associated weakness or neurologic findings. Due to her history of rheumatoid arthritis, her primary care physician advised a sooner follow-up with Rheumatology for subacute RA flare with her new knee pain. Four months later, the patient returned to her primary care physician after seeing her rheumatologist with unchanged tingling of her bilateral hands and feet and right knee pain.
She reports that her symptoms have caused her to fall twice since the last evaluation. She also notes some intermittent loss of control of her hands, causing her to drop trays of food at times. Due to her persistent and progressive symptoms, she was advised to obtain magnetic resonance imaging of her brain, cervical, thoracic, and lumbar spine. Imaging was significant for mild-to-moderate degenerative changes throughout the spine without spinal stenosis (Figure 1 and 2).

Figure 1 Multilevel spinal stenosis was noted in the sagittal view of the cervical spine.

Figure 2 Spinal stenosis and disc disease of the cervical spine.
Regardless, the patient was referred to Neurosurgery for further evaluation.
Neurosurgery saw the patient, and clinical presentation was correlated with imaging. The patient was diagnosed with cervical myelopathy due to severe ossification of the longitudinal ligament. And due to the severity of her sensory and motor symptoms, surgical intervention was recommended. During her C2 to C7 laminectomy with decompression and fusion, the patient was noted to have extensive OPLL than appreciated on imaging.
Upon reflection of this case, this patient had classic features of degenerative cervical myelopathy, specifically OPLL- widespread symptoms of pain, discomfort, tingling, neurologic deficits, and gait disturbances beginning in the fifth to sixth decade of life [1,7]. OPLL is more common in women and the Asian population; this patient is Vietnamese [8].
The posterior longitudinal ligament is essential in the stabilization of the spinal column. When it develops calcifications, it becomes thickened and can lead to spinal cord compression. Compression of the spinal cord will cause myelopathy and the possible symptoms, as noted above. Insidious and chronic symptoms of multiple levels of neurologic deficits should cause high clinical suspicion for myelopathy. Computed tomography (CT), can secure the diagnosis as plain radiography is not as sensitive during its early stages [7,9,10].
Conservative treatment such as monitoring, activity modification, and pain control can be beneficial early in its course [7,8,11]. But, the mainstay of treatment for OPLL is surgery and is strongly considered if the disease has progressed to motor involvement. The goal of surgery is to halt further neurological deterioration. Myelopathic symptoms are not guaranteed to improve.
Unfortunately, due to the rarity of OPLL as a DCM, it is rarely named on imaging, lumping its radiographic findings under the umbrella of degenerative changes. Compared to nervespecific radiculopathy, the widespread and vague symptoms of myelopathy are not often referred to surgical consultation. And surgeons, with their experiences in the operating room, are perhaps the best equipped to correlate symptoms, imaging, and pathology. Since patients are not often referred for consultation to surgical specialties without a diagnosis that explains their symptoms, cases of myelopathy are more likely to be delayed. OPLL’s widespread, vague, and intermittent symptoms are causing spinal canal stenosis. The patient reported immediate relief of her paresthesia, knee pain, and muscle cramping postoperatively. Her sense of balance has improved, denying any new falls, and she is no longer dropping items.
DISCUSSION
Due to the chronicity and progressive nature of the patient’s symptoms, the imaging was obtained but with findings that did not correlate with her symptoms- findings of only degenerative disc disease. Despite this, the patient was referred to Neurosurgery, where the patient’s symptoms were associated with imaging (Figure 3),
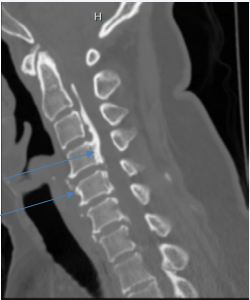
Figure 3 Calcification of the posterior longitudinal ligament, suggesting a diagnosis of OPLL.
and the diagnosis of ossification of the longitudinal ligament was made challenging to recognize, especially when not mentioned by name in radiographic results. However, OPLL is not uncommon and should be considered when extensive degenerative changes are noted on imaging. The degenerative changes in this patient’s imaging (Figures 1, 2 and 3), are rather extensive and warrant the need for “clinical correlation” with the specialist.
This case emphasizes the need for clinicians to review all ordered images and ensure that the crucial findings on imaging are consistent with what is reported. In addition, this case emphasizes the importance of “clinical correlation needed.”
CONCLUSION
With 50 to 60 percent of adults experiencing neck and arm pain at some point, cervical radiculopathy and myelopathy are essential diagnoses to consider [11]. Degenerative changes, the presence of facet joints, pedicles, and spondylosis can obscure the diagnosis, but most pathology, specifically OPLL, is best diagnosed with plain radiography and computed tomography [9,10]. This case illustrates the importance of regularly checking the images and not relying only on the final radiology report and the importance of correlating symptoms with imaging. A comprehensive clinical history and correlation with imaging are crucial to reaching an accurate diagnosis. If symptoms are not suggestive of nerve-specific radiculopathy, degenerative cervical myelopathy should be added to the differential diagnosis and surgical consultation to correlate symptoms with imaging considered.








































































































































