Anemia in Anorexia Nervosa: The Best Way to Deal with it-An Overview of Literature
- 1. Maison de Solenn - Maison des Adolescents- Cochin Hospital, Paris Descartes University, France
- 2. Service d’Hématologie-Cochin Hospital, Paris Descartes University, France
Abstract
Objective: Anemia is a condition marked by a deficiency of red blood cells. It is also one of the more common haematological complications of Anorexia Nervosa (AN). More often it is a benign complication resolving itself with proper anorexia nervosa care and refeeding but several cases may require more specific therapeutics.
Method: A systematic literature overview was performed using MEDLINE, the Cochrane Library and hand searching of relevant journals.
Results: Etiology of anemia in patients with AN can be in one of five categories: bone marrow malfunction, deprivation anemia, hemolysis, loss of hemoglobin, or inflammation. A complete blood work is necessary to pinpoint the exact etiology. Anemia within anorexic patients can be a very serious complication depending on its severity and etiology.
Discussion: Guidelines for the proper care of anemia within AN are critically needed since it can be a serious condition within those patients depending on its precise etiology. Unfavourable outcomes are more likely to happen if the weight loss was quick or if there are other comorbidities. We propose that each patient with active AN have a complete blood work with CBC, MCV, serum haptoglobin and iron levels, blood type and rhesus blood group, CRP, sedimentation rate and a complete iron blood work. If everything comes back normal on both, then there is no need to check it again if there is no unusual event. Treatment of anemia within AN should not be limited to a symptomatic treatment, but might also include etiological treatment and transdisciplinary approach if needed.
Keywords
• Anorexia nervosa
• Malnutrition
• Anemia
• Etiology
• Haematological complication
Citation
Mamou G, Sider A, Bouscary D, Moro MR, Blanchet-Collet C (2016) Anemia in Anorexia Nervosa: The Best Way to Deal with it-An Overview of Literature. J Hum Nutr Food Sci 4(1): 1081.
ABBREVIATIONS
AN: Anorexia Nervosa; ANHIC: Anorexia Nervosa Hyperactivity-Induced Ischemic Colitis; BT: Blood Transfusion; BMI: Body Mass Index; BMN: Bone Marrow Necrosis; CBC: Complete Blood Count; GMT: Gelatinous bone Marrow Transformation; MCV: Mean Corpuscular Volume; NICE: National Institute for Health and Care Excellence; RBC: Red Blood Cells.
INTRODUCTION
Anemia is a condition marked by a deficiency of red blood cells or of hemoglobin in the blood, resulting in pallor and weariness [1]. It is also known to be one the more common hematological complications of anorexia nervosa with a prevalence of 21-39% [2]. While it is most often due to bone marrow hypoplasia or gelatinous transformation in a malnutrition context [3-5], several other etiologies might be implicated that we should investigate prior to taking care of anorexic patients with anemia. Several studies examine a specific etiology of anemia within anorexic patients, but no systematic review has been conducted in this area. No clear guidelines had been proposed to the eating disorders specialist for the management of anemia within anorexia nervosa patients either. The primary objective of this article is to organize all rare etiologies of anemia within eating disorder patients that we should not overlook. The secondary objective is to propose simple guidelines to follow to help the physician to properly manage anemia within those patients depending on its etiology.
MATERIALS AND METHODS
The literature search was performed using the MEDLINE database, the Cochrane Library and hand searching of publication from 1939 to 2015. Eligibility criteria included all studies published between 1939 and 2015 written in English, French and German. We wrote a list of Medical Subject Heading (MeSH) terms that we used for all MEDLINE researches and used similar terms for the Cochrane Library and our hand searching. MeSH terms were anorexia nervosa, anemia, etiology, and hematological complication. We included 40 relevant articles in our review: fifteen systematic reviews, seventeen case reports, three non-US government financed basic research articles, one follow-up study, one case control study, one Letter to the British Medical Journal, one survival analysis and one historical article.
RESULTS
Etiology of anemia in Anorexia Nervosa (AN) patients can be in one of five categories: bone marrow malfunction, deprivation anemia, hemolysis, loss of hemoglobin, or inflammation (Table 1).
|
Table 1: Etiologies of anemia in Anorexia Nervosa. |
|||
|
Group of etiology |
Etiology |
Anemia characteristics |
Associated biology and clinical exam |
|
Bone Marrow Malfunction |
Bone Marrow Hypoplasia |
1st cause of anemia: 21-39% |
Leucopnia22-34% up to 75% of hospitalized patients |
|
Gelatinous Bone Marrow Transformation |
Frequency,underestimated |
Several lines affected. |
|
|
Bone Marrow Necrosis |
Rare. |
Pancytopenia |
|
|
Deprivation |
Iron deprivation |
Uncommon |
Low ferritin (might be normal) |
|
Folate / Cobalamine deprivation |
Extremely rare |
Low reticulocytes |
|
|
Hemolysis |
Refeeding Syndrome |
Rare |
Low haptoglobin level |
|
Drug-induced Hemolytic anemia |
Chlorpromazine |
normocytic, normochromic anemia with low serum haptoglobin |
|
|
Foot strike hemolysis |
Normochromic, normo- macrocytic anemia |
Low haptoglobin level |
|
|
Loss of hemoglobin |
Non occlusive mesenteric ischemia |
Rare |
Initial thrombopenia (rare) |
|
Anorexia Nervosa Hyper-activity Ischemic Colitis |
Extremely rare profound normochromic normocytic non-regenerative anemia |
Massive iron deficiency |
|
|
Somatoform or facticious disorder |
Extremely rare : Lasthénie de Ferjol syndrome. |
Lesions within thorough clinical exam (check for rectal prolapsus) |
|
|
Inflammation |
Anemia of inflammation and chronic disease |
microcyticanemia with low serum iron level |
Associated inflammatory disease :Crohn’s disease, etc. |
Anemia due to bone marrow malfunction
Bone marrow hypoplasia: Bone marrow hypoplasia is believed to be the first cause of anemia in AN patients [6-8] and is present in 39% of AN patients [5]. It is usually a moderate normochromic normocytic anemia, with acanthocytosis, anisocytosis and poikilocytosis. Ferritin and serum iron levels are generally normal, but ferritin can be augmented. It usually comes with leucopenia (22-34% of AN patients with bone marrow hypoplasia anemia, up to 75% within hospitalized patients), frequent neutropenia (17-38%) and lymphopenia (12%), and rare thrombopenia (5-10%) [8]. This anemia tends to reverse when refeeding is effective, with no long term consequences. Blood transfusion (BT) is never required, and no particular therapeutics are prescribed.
Gelatinous bone Marrow Transformation (GMT): GMT is characterized by bone marrow fat cell atrophy, focal loss of hematopoietic cells, and deposition of extra cellular gelatinous substances (mucopolysaccharides rich in hyaluronic acids) [9]. Prevalence of this condition is likely far underestimated since the myelogram is not systematic in AN patients; Abella et al., in 2002 reported that 50% of their AN patients had GMT, which would make it the first etiology of bone malfunction anemia in their AN population [5]. As of today, pathogenicity of GMT is not completely elucidated, but it is believed that the gelatinous deposits in the bone marrow cover for the secondary lack of adipocytes due to severe catabolism in AN and starvation [10]. The anemia is normochromic, normocytic and usually moderate but may require BT because of a higher risk of multi-visceral failure [11]. Severity of the anemia has proven to be correlated with the amount of weight loss [5]. Just like bone marrow hypoplasia, several lines are usually affected, GMT being the continuum of bone marrow hypoplasia in a malnutrition context [9,10]. G-CSF and erythropoietin treatment may be a good therapeutic to propose along with the correction of the nutrition deficiency, as it seems to decrease the need for hospitalization, thus reducing the costs of healthcare as well [11].
Bone marrow necrosis: Bone marrow necrosis (BMN) has been described in patients with AN by Smith et al., in 1984 [12]. Its mechanism is not completely elucidated, but it seems that it is the result of bone marrow hypoplasia and GMT plus another factor such as an infection or a sudden lack of nutrient. Others posit that it is caused by tissue hypoxia following microcirculation failure [13]. The anemia is normocytic and normochromic, and it is always accompanied by thrombopenia and leucopoenia. The examination of bone marrow shows non-identifiable pycnotic cells in greyish and orange matter, and disappearance of fat spaces. The bone tissue is usually preserved. The prognosis is far worse than GMT with multi-visceral failure.
Anemia due to deprivation
Deprivation anemia is sometimes believed to be common in patients with AN, but studies show that it is not the first etiology to look for within this population [2].
Iron deprivation: Anemia due to iron deprivation has been reported within AN patients but is an uncommon etiology [14]. Its physiopathology is very well known and it is characterized by a defect in hemoglobin synthesis resulting in small red blood cells and a decreased amount of hemoglobin [15], leading to a nonregenerative microcytic hypochromic anemia. It can be taken care of with oral iron supplementation.
Folate and / or vitamin B12 deprivation: Pernicious anemia is rare within AN patients but has also been reported [16]. Again, the mechanism at stake is well known, and it causes a characteristic megaloblastic anemia with ineffective erythropoiesis [17]. It can be associated with a slight leucopoenia. Thrombopenia occurs only in case of folate deficiency. Vitamin B1 and folate therapy has been proven effective.
Anemia due to hemolysis
Refeeding syndrome: Refeeding syndrome may occur in AN patients receiving artificial refeeding. Numerous mechanisms are implicated that lead, amongst other complications, to hypophosphatemia [18,19]. Hypophosphatemia can lead to intra red blood cells (RBCs) adenosine-tri phosphate depletion, along with intra RBCs 2,3-diphosphoglyceric acid depletion, modified RBCs affinity for oxygen resulting in decrease glucose utilization and increased lactate production. It results in the RBCs being rigid and very fragile, and in a microspherocytosis [20]. Due to those RBCs membrane abnormalities, hemolysis anemia is frequent during refeeding syndrome [21]; it is usually a normocytic anemia with low serum haptoglobin and low serum phosphorus (<0.5mg/dL) [20]. It is far easier to prevent refeeding syndrome than to treat it once it has occurred. The National Institute for Health and Care Excellence (NICE) has issued guidelines in 2006 on nutrition support in adults that should be the best way of preventing refeeding syndrome [18,22], but studies show that those guidelines might be an obstacle to providing adequate nutrition [23]. Systematic phosphorus supplementation is the only refeeding syndrome prevention therapeutic that physicians that deal with AN patients within clinks and in private practises all agree upon, but there’s no unity on which dosage to use [18,24]. Treatment of the refeeding syndrome includes supportive care and treatment of any electrolyte disorders (hypophosphatemia is not the only electrolyte disorder in the refeeding syndrome, but it is the one causing the haemolytic anemia) [24].
Drug-induced haemolytic anemia: How et al., reported two cases of AN patients who developed progressive haemolytic anemia during Chlorpromazine therapy in 1979 [25]. Haemolytic drug-induced anemia is common within hospitalized patients and not only AN patients, and this etiology of anemia should not been overlooked. More recently, Olanzapine has been proposed as an adjunctive treatment of AN patients [26,27], and the drug is known to cause haemolytic anemia [28]. It induces a normocytic, normochromic anemia with low serum haptoglobin and the treatment consists of stopping the administration of the implicated drug as soon as possible.
Foot strike hemolysis: Exercised-induced hemolysis is a well-known phenomenon that was first described in 1943 in cross country runners [29]. Patients with eating disorders are frequently engaged in excessive sports or physical activities. Persistent and severe hyperactivity is frequently associated with AN and a few biological explanations are being studied that implicate the low serum leptin level [30]. Physical hyperactivity can lead to foot strike haemolytic anemia (normocytic, normochromic, low haptoglobin level) in AN patients because of repeated foot trauma, especially since their skin is far thinner than those of marathon runners. Treatment of physical hyperactivity is not standardized and requires a multidisciplinary approach. Neuroleptics such as olanzapine or cyamemazine might be a good option, some studies also cite serotonin reuptake inhibitors or opioid antagonists but there is no clear recommendation about it as of today [31,32].
Anemia due to loss of hemoglobin
Non occlusive mesenteric ischemia: Reported by Yamada et al., in 2001 within an anorexia nervosa patient, non-occlusive mesenteric ischemia is well known amongst patients who just had a heavy surgery [33-36] and patients undergoing chemotherapy [37]. It is a low flow syndrome of mesenteric circulation brought by heart failure, hypotension, or hypovolemia, followed by vasoconstriction [33]. Blood can be found in stools but it is sometimes difficult to catch the right moment. The anemia is caused by loss of hemoglobin; it is usually normocytic normochromic anemia, and might be accompanied by iron deficiency due to chronic blood loss.
Anorexia Nervosa Hyperactivity-induced Ischemic Colitis (ANHIC): This new entity was first reported by Blanchet-Collet et al., in 2015. Marathon induced ischemic colitis is a well know phenomena causing multiple small colitis ischemia within long distance runners [38]. Blanchet-Collet et al., reported the case of a young patient suffering major hyperactivity in anorexia nervosa [Case report has been accepted Eating and Weight Disorder journal]. She had profound anemia and required multiple blood transfusions. All tests were normal and the anemia seems to have been caused by a phenomenon resembling the marathon induced anemia because of her hyperactivity. ANHIC may be very underestimated within patients suffering from hyperactivity. It causes a profound normochromic normocytic non-regenerative anemia with massive iron deficiency.
Somatoform or factitious disorders: Factitious anemia has been reported, and is a great challenge for physicians [39-41]. French physician Jean Bernard described Lasthénie de Ferjol syndrome in 1967; it consists of a factice anemia obtained by repeated self-mutilation of iterative blood donation. Loloum et al., made the parallel between Lasthénie de Ferjol and AN as early as 1985, and it should be brought up when no other etiology fits [42]. The anemia is microcytic, hypochromic, and a thorough clinical exam should reveal skin or mucosa damage (especially rectal prolapse).
Anemia of inflammation and chronic disease
Anemia of inflammation can easily be confused with iron deprivation anemia because it is a microcytic anemia with low serum iron level since inflammatory and chronic disease interferes with the body’s ability to use stored iron and absorb iron from food in the digestive tube [43]. Any patient suffering from anorexia nervosa could also have a chronic inflammatory disease causing an anemia of inflammation; a link between anorexia nervosa and Crohn’s disease has already been reported by several authors [44,45] and it is legitimate to suppose that others chronic inflammatory diseases could be linked to anorexia nervosa.
DISCUSSION
Anemia is undoubtedly a common and multifactorial complication of anorexia nervosa. In most cases it presents as a moderate, transitory, and asymptomatic anemia and would eventually correct by itself with proper care for AN, particularly with appropriate and progressive refeeding. Still, because of the potential severity of some anemia within anorexia nervosa patients, it seems essential to look for it during systematic exams of those patients. Many anemia cases in AN patients have been misdiagnosed as bone marrow hypoplasia or iron deprivation anemia. No one can predict how a mild and asymptomatic anemia will evolve.
Unfavourable outcomes from anemia in AN patients is related for the most part to its etiology and might have no direct link with the patient’s BMI (Body Mass Index). That would mean that patients that are the most at risk of a major hematologic complication are not necessarily the ones with the lowest weight and/or BMI. It seems that the speed of the weight loss is far more critical than the BMI concerning the outcome; the quicker you lose weight, the more the complications may be severe. Somatonutritional condition and psychiatric comorbidity should not be taken lightly since it is often proper treatment for anemia that implicate the treatment of some comorbidities; the proper treatment for a haemolytic anemia might implicate treating along a refeeding syndrome, to stop administering a responsible medicine, or initiating (or intensifying) a psychiatric therapy for hyperactivity in a foot strike hemolysis. The same thing applies for patients suffering from ANHIC or somatoform or factitious disorder.
On the other hand, it still happens today that patients with severe AN are hospitalized in haematology for exploration of an anemia, and where the AN diagnosis is completely overlooked. That can’t be an acceptable management of those patients since in most cases these cases of anemia will be resolved themselves with proper and progressive refeeding. Deep and invasive exploration of anemia within AN patients is sometimes recommended, but only after an examination. Clinics should always prevail on mild, asymptomatic anemia.
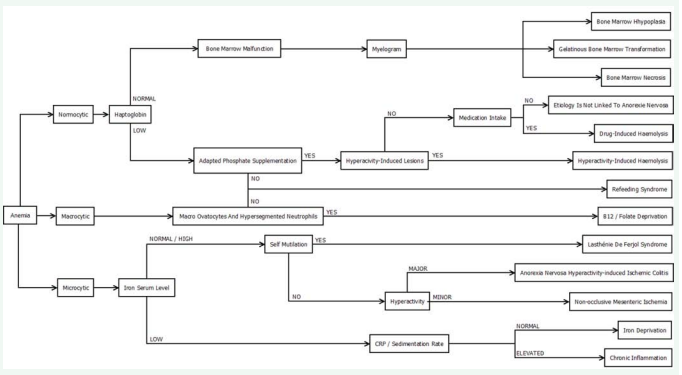
Figure 1 proposes a simple algorithm to help determine the etiology we should suspect when dealing with anemia in AN patients using only mean corpuscular volume (MCV), serum haptoglobin level, serum iron, C-reactive protein serum level and in some cases a myelogram.
Figure 1: Etiology chart of anemia in Anorexia Nervosa.
When dealing with a normocytic anemia with normal serum haptoglobin level, a myelogram is the only way to differentiate bone marrow hypoplasia, gelatinous bone marrow transformation and bone marrow necrosis.
Bailly et al., suggested in 1994 that bone marrow necrosis may predominate when interruption of nutrient delivery is sudden, where GMT may predominate when interruption of nutrient delivery occurs more slowly [4,12]. Abella et al., showed that there is an excellent correlation between cytologic and histologic findings, suggesting that bone marrow aspiration would be clearly sufficient [5]. They also showed in the same study than bone marrow lesions were associated with the severity of the ponderal loss. Still all these authors agree on the fact that these lesions tend to reverse with proper nutrition only, and we suggest that bone marrow aspiration should not be considered on a diagnosis basis for anemia in AN patients. Moreover, those patients often have haemostasis malfunction and bone marrow aspiration can be a very delicate process that might lead to massive bleeding.
We believe that many anemia within those patients are either from multifactorial etiologies or other uncovered physiopathology. A normocytic normochromic anemia within a patient could theoretically be the result of a mixed iron and B12/ folate deprivation. It is difficult to imagine all the unknown and intricate etiologies of anemia within AN because of the complexity of the physiological changes within those patients, including nutritional deficiencies, hormonalvariations and multiorgan failures. For example, deficit in erythropoietin associated with renal insufficiency is not rare in anorexic patients, and androgen levels reduction could be also implicated in anemia within AN patients. It seems that several recently discovered etiologies of anemia within AN like foot strike hemolysis, non-occlusive mesenteric ischemia or ANHIC were known etiologies for anemia within another patient population. Thus, it seems legitimate to propose that other rare etiologies of anemia within AN patients might be discovered by first studying rare etiologies of anemia within other undernourished patients like patients undergoing chemotherapy or with chronic digestive or renal disorder leading to malnutrition.
No clear guidelines have been issued concerning the management of anemia within AN patients, and in particular within anorexic inpatients whose initial clinical condition could be uncertain. We believe that guidelines are sorely needed since it is a very common complication of this condition and, as we just exposed, may lead to a very unfavourable outcome. From our review of literature we can see that anemia due to AN is one of five big etiology groups: bone marrow malfunction, blood deprivation, hemolysis, loss of hemoglobin or inflammation. It is easy to know which kind of anemia we are dealing with by taking a blood sample and a thorough clinical exam. Thus, we propose that each in-patient with active AN should have a complete blood work with CBC, MCV, serum haptoglobin, blood type and rhesus blood group, CRP, sedimentation rate and a complete iron blood work (serum iron level, ferritin and transferrin saturation level). B12/folate deprivation is really rare and their serum dosage is not recommended in first intention.
If everything comes back normal after several CBCs within a few weeks, then there is no need to check the CBC again if global somato-nutritional and psychiatric evolution is reassuring and if there is no special medical event.
CONCLUSION
Anemia could be a transient and benign but conversely a serious and life-threatening somatic complication in anorexia nervosa. Different anemia etiologies and characteristics should be known by physicians in order to provide adequate care to anorexic patients and to avoid dramatic diagnostic or therapeutic mistakes. The treatment of anemia within AN patients is a three pane one: a symptomatic treatment of the anemia, implicating sometimes blood transfusion in extreme medical conditions (justifying the realization of a blood type and rhesus blood group at the beginning of the treatment), an etiological treatment of the anemia, and a transdisciplinary approach with psychological or psychiatric support.
REFERENCES
1. Oxford D. Paperback Oxford English Dictionary, in Paperback Oxford English Dictionary: 7th Edition. 2013, Oxford University Press.
6. Pearson HA. Marrow hypoplasia in anorexia nervosa. J Pediatr. 1967; 71: 211-215.
7. Lampert F, Lau B. Bone marrow hypoplasia in anorexia nervosa. Eur J Pediatr. 1976; 124: 65-71.
13. Kiraly JF 3rd, Wheby MS. Bone marrow necrosis. Am J Med. 1976; 60: 361-368.
14. Evans JCG. Anorexia Nervosa. The Lancet, 1939. 233: 268-269.
15. Provan D. Mechanisms and management of iron deficiency anaemia. Br J Haematol. 1999; 105: 19-26.
16. Lambert M, B Boland. Hematological Complications. Eur. Eat. Disorders Rev. 2000; 8: 158-163.
17. Pruthi RK, Tefferi A. Pernicious anemia revisited. Mayo Clin Proc. 1994; 69: 144-150.
21. Porter RS. The Merck Manual. 19th ed. 2011. 3754.
22. NICE National institute for Health and Care Excellence. Nutrition support in adults, in Clinical Guidelines. 2006.
24. Kraft MD, Btaiche IF, Sacks GS. Review of the refeeding syndrome. Nutr Clin Pract. 2005; 20: 625-633.
27. Jensen VS, Mejlhede A. Anorexia nervosa: treatment with olanzapine. Br J Psychiatry. 2000; 177: 87.
28. Lilly E. ZYPREXA (Olanzapine) prescribing information. 1997.
43. U.S Department of Health and Human Services. Anemia of inflammation and Chronic Disease. 2013.