Anti-Obesity and Lipid-Lowering Properties of Alpha-Lipoic Ac
- 1. Department of Exercise and Nutrition Sciences, School of Public Health and Health Professions, University at Buffalo, Buffalo, NY, 14214, USA
Abstract
Reducing the prevalence of obesity and obesity-related metabolic disturbances is the foremost priority of global health care initiatives. Sustained lifestyle modifications to diet and daily activity patterns will be the foundation of effective strategies to reduce obesity and improve public health. In addition to diet and exercise strategies, supplementation of nutraceuticals, naturally occurring bioactive compounds capable of eliciting specific health responses, may offer a safe and convenient approach to reduce metabolic disease risk factors. Alpha-lipoic acid (α-LA), an 8-carbon dithiol compound that is an essential cofactor in mitochondrial respiration, is notable amongst nutraceuticals as it offers a wide array of metabolic benefits with purported antiobesity, glucose lowering, insulin sensitizing, and lipid-lowering effects. This review summarizes the pre-clinical and clinical evidence supporting the anti-obesity and lipidlowering effects α-LA and highlights the potential mechanisms involved.
Keywords
• Alpha-lipoic acid
• Lipids
• Lipoproteins
• Lipogenesis
Citation
Carrier B, Rideout TC (2013) Anti-Obesity and Lipid-Lowering Properties of Alpha-Lipoic Acid J Hum Nutr Food Sci 1(1): 1002.
OBESITY AND RELATED METABOLIC COMPLICATIONS IN THE US
Over the past twenty years, the global population has experienced a dramatic increase in obesity and obesity-related metabolic complications. In the U.S., 35.7% of adults and approximately 17% of adolescents from ages 2-19 years of age are considered obese [1]. Obesity and obesity related metabolic disturbances have reached epidemic proportions, particularly in adolescent populations [2,3]. Since 1980, the prevalence of childhood obesity has almost tripled in the U.S., forecasting a major obstacle to the health of future populations [4]. The worldwide increase in obesity has been found to be associated with the widespread availability of rather inexpensive, energy dense foods high in saturated fat, sugar, and refined carbohydrates, the increase in high fructose corn syrup ingestion, and a shift to a more sedentary lifestyle due to technological advancements [5-7]. Diet and lifestyle factors are important determinants of MetSyn, a constellation of risk factors that increases the risk of cardiovascular disease (CVD) by 50-60% [8]. Available evidence indicates that in the U.S., approximately 20-30% of the adult population (~47 million people) has one or more MetSyn risk factors including increased blood pressure, increased waist circumference, and hypertriglyceridemia [9,10]. Considering the high incidence of obesity and related metabolic complications, it is imperative to identify safe and effective therapeutic options. Even in the face of genetic predisposition, lifestyle modifications to physical activity and dietary patterns can be effective in weight reduction and alleviating multiple disease risk factors. However, long-term compliance to drastic changes to diet and daily activity patterns is often difficult and unrealistic given the hectic lifestyle of modern societies. Health-promoting nutraceuticals - naturally occurring bioactive compounds capable of eliciting targeted molecular responses at the cellular level – may be an effective and convenient strategy to improve overall health and reduce disease risk. Furthermore, nutraceutical compounds could prove to be a powerful alternative to pharmacotherapy, as they are relatively safe, cost effective, and possess the ability to modulate specific, and sometimes multiple, molecular targets [11].
ALPHA-LIPOIC ACID-STRUCTURE, SOURCE, AND METABOLISM
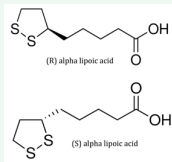
One nutraceutical with a multiple array of potential clinical applications particularly advantageous for obesity-related metabolic abnormalities is alpha lipoic acid (α-LA) [11]. α-LA is an 8-carbon dithiol compound synthesized in hepatic mitochondria from octanoic acid. It can exist in the oxidized form, α-LA, or the reduced form, dihydrolipoic acid. α-LA acid contains a chiral carbon and therefore exists as both an R+- and S- enantiomeric form (Figure 1) [12].
Figure 1: Structure of R and S alpha lipoic acid enantiomeric forms.
α-LA is a necessary cofactor for mitochondrial α-ketoglutarate dehydrogenase and pyruvate dehydrogenase, both important enzymes in cellular energy metabolism [13]. In addition to de novo synthesis, α-LA can be absorbed from plant and animal-based dietary sources including red meat, liver, kidney, heart, spinach, broccoli, tomatoes, and brussel sprouts, although in minor amounts [13]. While the mechanism of absorption is not clearly defined, there is evidence to indicate that α-LA may be absorbed through multiple transporters including the monocarboxylic transporter [14] and the sodium-dependent multivitamin transporter [15]. Due to these multiple absorptive routes, α-LA absorption may be affected by substrate competition and subject to transcriptional and post-transcriptional regulation of specific carrier proteins [13]. Treichert et al. (1998) demonstrated that 20-40% of a 200 mg R+ α-LA acid supplement was absorbed in human subjects, and that absorption was significantly decreased when ingested with food, indicating potential substrate competition between α-LA and other nutrients [16]. Evidence suggests that the R+ enantiomer is preferentially absorbed over the S-enantiomer, though it is equally likely that the R+ form has a greater postabsorptive retention than the S-form [12]. Plasma levels of the R+ enantiomer have been found to be 40-50% greater than the S enantiomer following ingestion of a 600 mg racemic mixture [13]. Tissue accumulation of α-LA is transient and is known to accrue in limited quantities in the liver, heart, and skeletal muscle [13]. Intracellular α-LA is quickly oxidized to produce approximately 12 different metabolites. Furthermore, there exists a separate glycine conjugation pathway that competes for metabolism of α-LA in animals that does not appear to occur in humans [17]. Overall, pharmacokinetic studies suggest that α-LA is rapidly absorbed and cleared from the plasma due to tissue uptake or renal excretion [18]. Relatively little is known regarding the tissue distribution or retention of α-LA or its metabolites [19]. Given its apparent rapid oxidation and transient tissue accumulation, the vast array of metabolic effects of α-LA is remarkable.
ANTI-OBESITY RESPONSES TO ALPHA-LIPOIC ACID
Although the precise mechanisms are not completely defined (see below), α-LA has been shown to exhibit a weight-loss effect and an attenuation of weight gain in both animals and humans. Sprague-Dawley rats fed a high fat diet supplemented with 0.25 or 0.5% α-LA demonstrated a 10% and 21% attenuation of weight gain, respectively, compared to a high fat-fed control group. This reduction in weight gain was attributed to decreased feed intake, supporting a well-characterized anorectic effect of α-LA [20]. This anorectic effect of α-LA is most pronounced during the initial 2 weeks of supplementation and gradually dissipates over the duration of supplementation [21]. α-LA supplementation (0.5%) has also been shown to reduce body weight in Wistar rats by 30% with an associated reduction in epididymal and perirenal fat mass [22].
Although studies are limited, there is clinical support of an anti-obesity effect of α-LA acid. In a double-blind, placebocontrolled intervention, Koh et al. (2011) randomized 360 obese subjects to a placebo, 1200 mg or 1800 mg α-LA group for 20 weeks. After observing a modest (2.1 %) weight loss in the 1800 mg α-LA group compared with the placebo-controlled group [23], the authors suggested that α-LA supplementation may be an effective adjunctive therapy for obesity. For instance, α-LA may prove to be a suitable adjunct therapy to support weight loss with effective diet and/or exercise initiatives. To date, although combination α-LA/exercise interventions have shown to have promise in improving insulin sensitivity [24], there have been no studies conducted to examine if α-LA enhances weight loss in conjunction with exercise.
Carbonelli et al. (2010) observed a decrease in body fat mass (~7-9%), BMI (~3 points), and waist circumference (~8 cm) in obese and pre-obese subjects supplemented with 800 mg of α-LA per day for 4 months [25]. In a preliminary study to assess α-LA as a supplement to combat the antipsychotic-induced weight gain observed in schizophrenia, Ratliff et al. (2013) reported significant weight loss (?2.2 kg ± 2.5 kg) in 12 non-diabetic schizophrenia patients consuming 1200 mg/α-LA over ten weeks. Overall, these human studies provide promising evidence for the use of α-LA as an effective anti-obesity agent in overweight patients. However, additional controlled human studies are required to fully define the clinical utility, efficacy, and safety of α-LA as a weight loss supplement.
LIPID-LOWERING RESPONSES TO ALPHA-LIPOIC ACID
In addition to weight reduction (or perhaps because of), α-LA has been purported to improve plasma lipid profile, including reductions in plasma LDL-C, total cholesterol, and triglycerides (TG). It is currently unclear whether these lipid-lowering responses are secondary to a reduction in feed intake or weight loss, or if they are the product of a more direct molecular effect of α-LA.
Evidence from multiple animal models suggests a lipidlowering response to α-LA supplementation. Sprague-Dawley rats fed a high fat diet with 0.5% α-LA demonstrated a reduction in total blood lipids (21.3%), TG (31.9%), total cholesterol (20.1%), LDL-cholesterol (41.1%), and free fatty acids (33%) relative to the rats fed the high fat diet alone [26]. Another study, which examined the effects of different dosages of α-LA (0, 1, 2.5, and 5 g/kg) in Sprague-Dawley rats on plasma lipid profile reported reductions in TG (68.5%), total cholesterol (25.8%), and non-esterified fatty acids (45%), although no dose-response relationship was found [27]. Similar attenuation of plasma total cholesterol (31%) has also been found in New Zealand White rabbits fed a cholesterol diet supplemented with 4.2 mg α-LA / kg body weight compared with rabbits fed a high cholesterol diet only.
In addition to lipid reductions in the blood, α-LA has also been shown to modulate intracellular lipid storage patterns. Butler et al. (2009) reported a reduction in hepatic total lipid (26.8%) and TG concentrations (27%) in ad libitum-fed Zucker rats supplemented with 2.4 grams α-LA/kg BW for 5 weeks [21]. Results of Seo et al. (2012) support modulation of hepatic lipids in response to α-LA with reductions in hepatic total cholesterol (41.1%) and total lipids (21.1%) in Sprague-Dawley rats supplemented with 0.5% α-LA [20]. These pre-clinical results may highlight the potential value of α-LA as a supplement to offer protection against non-alcoholic liver disease. This disorder, with an alarming prevalence (>80%) in obese individuals, is characterized by multiple hepatic pathologies associated with excessive accumulation of hepatic TG and hepatic steatosis and currently has limited treatment options [28].
Limited evidence from human studies suggests that α-LA may be an effective lipid-lowering compound [29]. A short-term α-LA administration study by Zhang et al. (2011) reported significant reductions in plasma free fatty acids, TG, total cholesterol, LDLcholesterol, oxidized LDL-cholesterol, and VLDL-cholesterol in obese subjects with impaired glucose tolerance that were treated with 600 mg of α-LA intravenously for 2 weeks [30]. Results from this study suggest that α-LA may have lipid-lowering properties independent of weight loss, at least when provided intravenously. Masharani et al. (2010) observed reductions in plasma TG (28%) and larger, more buoyant LDL-particles in six lean subjects with polycystic ovary syndrome after receiving controlled-release α-LA capsules (600 mg) twice daily for sixteen weeks [31]. As study subjects were placed on a weight-maintaining diet, results from this small-scale study lends support that enterallysupplied α-LA can reduce plasma lipids in the absence of weight loss. On the other hand, a case study of five overweight/obese schizophrenic patients by Kim et al. (2008) reported weight loss (3.16 kg) and mean reduction in total cholesterol of 8% and a tendency toward lower LDL-C and higher HDL-C following 12 weeks of α-LA supplementation at 1200 mg/day [32]. Results of this study may be typical of the lipid lowering responses that would be expected in the context of relevant weight reductions following α-LA supplementation.
Conversely, other human intervention studies have reported no effect of α-LA on lipid profile. Diabetic end-stage renal disease patients on hemodialysis receiving 600 mg α-LA per day for 12 weeks exhibited no differences in total cholesterol or oxidizedLDL compared with the control group [33]. In a similar patient population, a double-blinded, randomized, placebo-controlled clinical trial did not detect any change in plasma lipid profile following 600 mg α-LA supplementation for 8 weeks compared to placebo [34]. In 62 patients with age-related macular degeneration randomly assigned to a placebo (n=30) or a 600 mg α-LA capsule (n=32), Sun et al. (2012) failed to detect α-LAinduced changes in plasma lipids versus placebo [35]. No weight change was reported in this study. Finally, in the previously mentioned study by Koh et al. (2011), even after weight loss, no change total-C, HDL-C, or TG was reported in 360 obese individuals randomized to placebo, 1200 or 1800 mg/ α-LA/d [23].
Overall, the clinical trial database is limited and inconsistent in characterizing the lipid-lowering effects of α-LA. Few intervention studies have been specifically designed to examine lipid responses as a primary study endpoint. In addition to establishing the expected magnitude of lipid-reductions following different doses of α-LA, clinical studies are required to specifically examine if α-LA improves blood lipids in the absence of reduced feed intake and weight loss.
ANTI-OBESITY AND LIPID-LOWERING MECHANISMS OF ALPHA LIPOIC ACID
Strong pre-clinical evidence and less robust clinical data suggests that α-LA exerts anti-obesity and hypolipidemic effects, however, the contributing mechanisms that underlie these lipid responses are not completely understood.
Mechanistic studies suggest that α-LA may directly and/or indirectly modulate the expression of a whole host of master switches that alter the transcriptional and translational activity of cellular targets that control feed intake, energy homeostasis, fat synthesis, fat oxidation, and hepatic cholesterol clearance.
One such master switch is 5’ AMP-activated protein kinase (AMPK). AMPK is stimulated by a decrease in cellular ATP and subsequently activates catabolic (energy yielding) pathways and inactivates anabolic (energy utilizing) pathways. AMPK is known to integrate hormonal and nutrient signals in the hypothalamus and thus has a functional role in regulating feeding behavior and whole-body energy expenditure [36,37]. Previous work suggests that α-LA-induced modulation of AMPK in both central and peripheral tissues plays a major role in mediating the anti-obesity and lipid-lowering effects of α-LA [38,39]. In an elegant rodent study conducted by Kim et al. (2004), dietary supplementation of α-LA suppressed hypothalamic AMPK activity and caused an up regulation of whole-body energy expenditure and a decrease in food intake, manifesting in a profound weight loss [38]. The role of AMPK in mediating these responses was verified upon activation of hypothalamic AMPK activity. In concert with the observed anorectic effect, α-LA acid was shown to stimulate whole body energy expenditure at least in part by up regulating the expression of uncoupling protein 1, a protein which functions to dissipate the proton electrochemical gradient in mitochondria and release this energy as heat. α-LA has also been shown to induce AMPK phosphorylation and activation in white adipose tissue [40], C2C12 myotubes [29], aortic tissue [41], skeletal muscle [42], and liver cells [43]. However, studies have highlighted a potential temporal effect of α-LA on AMPK activity, with peripheral activation evident in acute studies but not as apparent in long-term studies. In their examination of the effects of α-LA on muscle lipid accumulation in Wistar rats, Timmers et al. (2010) determined that there were no changes in AMPK activity in muscle after 8 weeks of α-LA supplementation and that the observed reduction in muscle lipid accumulation was likely secondary to the anorectic effect of α-LA [22]. Alternatively, results from in vitro studies suggest an acute response of α-LA on AMPK activity. In a study examining the effects of α-LA exposure in rat islets and MIN6 cells, exposure time of 15-90 min and 18-24h led to a dose-dependent increase in phosphorylation of AMPK and ACC [37].
Although α-LA appears to inhibit hypothalamic AMPK to promote reductions in feed intake, α-LA stimulation of AMPK activity in peripheral tissues such as skeletal muscle has been shown to directly inhibit fatty acid synthesis, while concomitantly increasing in β-oxidation of fatty acids [20,27,39]. Multiple studies suggest that the expression of the two ratelimiting enzymes in fatty acid synthesis, acetyl-CoA carboxylase (ACC) and fatty acid synthase (FAS), are reduced in response to α-LA supplementation [20,44]. Huong et al. (2008) observed a dose-dependent decrease in the activity and mRNA expression of FAS in Sprague Dawley rats fed 1, 2.5, and 5 grams of α-LA /kg body weight for twenty-one days [27]. These results were supported by results from Park et al. (2008) who observed reductions in hepatic ACC and FAS in Sprague Dawley rats fed 2.5 mg α-LA /kg body weight for 8 weeks. Reductions in lipogenic gene expression were also observed in a pair-fed group, but to a lower extent, suggesting that the responses were directly related to α-LA and not secondary to suppressed food intake [39]. Butler et al. (2009) also demonstrated a decrease in ACC 1 and 2 and FAS mRNA expression by 66, 52, and 74%, respectively in Zucker diabetic rats supplemented with 2.4 grams of α-LA /kg body weight [21]. Responses in the pair-fed group again suggested a direct molecular effect of α-LA acid on hepatic lipogenesis. The decrease in mRNA expression was also found to be associated with an inhibition of ChREBP, a known transcriptional regulator of lipogenesis, suggesting a possible alternative mechanism for α-LA. Additionally, α-LA has been found to modulate SREBP1c expression, a transcriptional regulator of lipogenic enzymes that is stimulated by insulin. The previously mentioned study by Park et al. (2008) observed a decrease in hepatic SREBP1c expression in Sprague-Dawley rats fed a high fat diet supplemented with 0.5% α-LA [39]. Furthermore, Castro et al. (2012) recently reported that α-LA was effective in restoring basal SREBP1c expression in fructose-fed rats [45]. Reductions in SREBP1c expression in response to α-LA supplementation may be associated with hormonal changes as α-LA has been shown to decrease plasma insulin concentrations, a known inducer of SREBP1c [46,47]. Therefore, reductions in blood and tissue lipids following α-LA may be secondary to decreases in plasma insulin concentrations.
Concomitant with a decrease in hepatic lipogenesis, α-LA has been found to modulate hepatic β-oxidation of fatty acids [20,26]. A previous report linked protection against high fat dietinduced dyslipidemia in C57BL/6 mice fed α-LA (0.1%) to an up regulation of the mRNA expression of hepatic genes regulating β-oxidation, including carnitine palmitoyltransferase 1 (CPT1), peroxisome proliferator-activated receptor alpha (PPARalpha), and acyl-CoA oxidase (ACOX); however, no changes were found in mRNA expression of genes related to fatty acid synthesis [26]. In mediating up-regulation of fatty acid oxidation in the liver, α-LA may protect against a high fat load by increasing oxidation of exogenous fatty acids for energy. Lee et al. (2005) provided additional evidence of α-LA–induced β-oxidation in Otsuka Long Evans Tokushima Fatty rats supplemented for 3 days with 0.5% (wt/wt) racemic α-LA. The authors reported that α-LA supplementation decreased TG accumulation and increased β-oxidation of fatty acids in skeletal muscle. ACC phosphorylation was also increased in the α-LA supplemented group, indicating an inhibition of fatty acid synthesis [47]. Finally, Yang et al. (2008) also reported that lipid reductions (total-C, LDL-C, and TG) in response to 0.1% α-LA supplementation were associated with an increase in hepatic β-oxidation and free radical scavenging systems [26].
SAFETY OF ALPHA-LIPOIC ACID
The short and long-term safety and toxicity of parenteral and enteral α-LA supplementation has been examined in both animals and human subjects. In general, oral doses of up to 1200 mg α-LA /day have been shown to be well tolerated with only minor side effects, particularly with parenteral formulations >600 mg/d [48]. α-LA has been approved as an over-the-counter treatment for diabetic polyneuropathy in Germany for >50 years [49]. Post-marketing monitoring of adverse drug reactions suggest that α-LA is well tolerated with a low rate of reported adverse reactions [50]. Ziegler and colleagues have conducted both shortterm (5 weeks) and long-term (4 years) studies to examine the effect of α-LA on sensory symptoms in diabetic patients with distal symmetric polyneuropathy. These studies also included a secondary analysis of safety and adverse events. The shortterm, multicenter, randomized, double-blind, placebo-controlled trial examined doses of 600, 1200, and 1800 mg α-LA/d [51]. Although the low dose of α-LA had a favorable safety profile, a dose-dependent increase in nausea, vomiting, and vertigo was reported with higher doses. The long term placebo-controlled, randomized study examined the efficacy and safety of a daily dose of 600 mg α-LA for 4 years in 400 subjects [51]. Although treatment tolerability was assessed as similar between the α-LA and placebo groups, the rates of serious adverse events were higher on α-LA treatment (38.1%) versus placebo (28.0%) even though only two α-LA and one placebo subject dropped out of the study due to adverse events.
SUMMARY AND CONCLUSIONS
In summary, reports from existing animal and human studies suggest that α-LA possesses an impressive array of metabolic effects that may offer protection against obesity-related metabolic disturbances. Mechanistic studies support the idea that α-LA exerts anti-obesity and lipid-lowering effects through multiple mechanisms. Modulation of hypothalamic and peripheral AMPK appears to play a particularly important role by regulating food intake, reducing lipogenesis, increasing β-oxidation of fatty acids, and enhancing whole-body energy expenditure. Although limited data from human studies suggest that α-LA has potential clinical utility, additional properly controlled randomized studies are required that are specifically designed to examine weight loss or blood lipids are required. Also, more studies are required to determine the most effective and safe dose of α-LA as existing human studies have been conducted with wide ranging doses and formulations.
ACKNOWLEDGEMENTS
We would like to thank Dr. Mulchand Patel and Dr. John X. Wilson for their assistance in preparing this review.