Reversal of Type 2 Diabetes in a 14 Year Old Post Pubertal Child using a Low Calorie Liquid Replacement Diet and a GLP1 agonist
- 1. Paediatric Dietitian & Team Lead, Hampshire Hospitals NHS Foundation Trust, UK
ABSTRACT
Type 2 diabetes is an aggressive form of diabetes in children and young people with the risk of early onset micro and macrovascular complications. The intervention of a reduced calorie liquid diet and treatment with a GLP1 agonist to try to reverse type 2 diabetes in a 14-year-old patient is described.
CITATION
Allmark G, Paye J, Houghton V, Williams E (2023) Reversal of Type 2 Diabetes in a 14 Year Old Post Pubertal Child using a Low Calorie Liquid Replacement Diet and a GLP1 agonist. J Hum Nutr Food Sci 11(1): 1156.
BACKGROUND
Our patient was diagnosed with type 2 diabetes at the age of 10 years and has a strong family history of type 2 diabetes. She had an earlier puberty with menses at aged 10 years.
At the age of 14 years, she had poorly controlled Type 2 diabetes. Her BMI was high, greater than 30kg/m2 (Figure 2) and her glycaemic control was poor with high HbA1c levels (Figure 3). Her treatment regimen comprised Metformin 1000mg twice daily, Degludec insulin 16 units daily and Novorapid insulin with all meals (total daily insulin dose approximately 0.6 Units/ kg/day). She was not taking her insulin reliably which made it difficult for the diabetes team to make changes to her treatment regimen and she was not carbohydrate counting thus the doses of Novorapid were determined based on previous experience only.
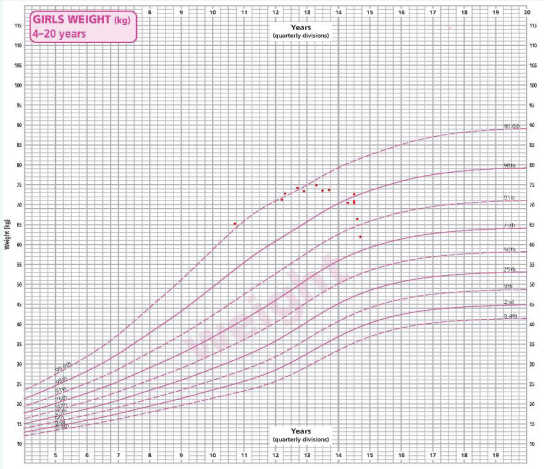
Figure 1 Weight history chart from outpatient appointments with the diabetes team Nov 2018-Sept 2022.
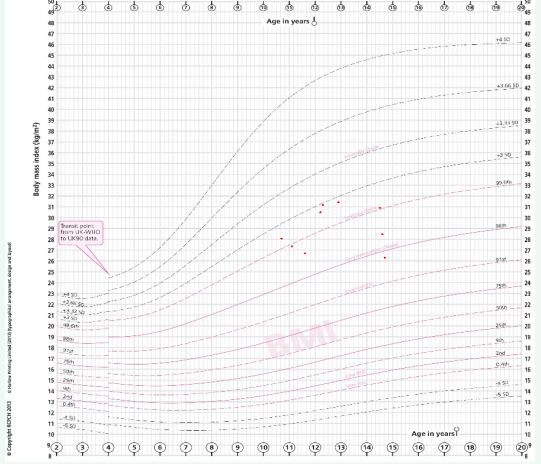
Figure 2 BMI history chart from outpatient appointments with the diabetes team Nov 2018-Sept 2022.
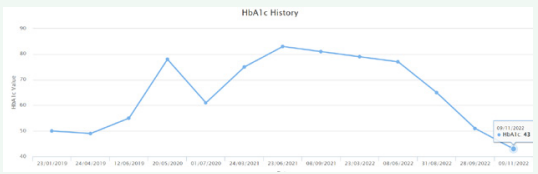
Figure 3 HbA1c history chart from outpatient appointments with the diabetes team Nov 2018-Sept 2022.
The intervention of a reduced calorie liquid diet and treatment with a GLP1 agonist to try to reverse her type 2 diabetes was proposed and discussed with our patient and her family. It was agreed that it would be safest for this intervention to be carried out as a hospital admission. This decision was based on our previous experience of a liquid diet intervention causing frequent hypoglycaemic episodes and it was also felt that our patient could be better supported as an inpatient to follow the plan. Both our patient and her parents were keen and committed to try this intervention.
Dietary intervention
A liquid dietary plan was created by the paediatric dietitian.
Due to our patient’s young age a calorie restriction of 1200kcal/ day proposed; this is not as low as adult based interventions (typically 800kcal/day).
The dietary plan consisted of 2 phases (appendix 1-adapted from Portsmouth hospitals version):
Phase 1 (weeks 1 and 2) - liquid shakes (supermarket own brand) + multivitamin supplements (over the counter)
Total 1200kcal/day
Phase 2 (weeks 3 to 6) - meal reintroduction + multivitamin supplements
- Week 3- introduce lunch (back at school)
- Week 4- introduce breakfast
- Week 5- introduce evening meal + snack
- Week 6- introduce 1 more snack Total 1400kcal/day
The family purchased the required liquid replacement shakes and the multivitamin tablets prior to the admission. A range of options for the shakes were provided by the dietitian and choices were made based on our patient’s preferred brand and flavouring.
GLP 1 Semaglutide intervention
The Semaglutide regimen was prescribed as per BNF guidelines
-Semaglutide 0.25mg subcutaneous injection once weekly for 4 weeks
-Semaglutide 0.5mg subcutaneous injection once weekly for 4 weeks
-Semaglutide increased to 1mg once weekly if required
Management during hospital admission
Our patient was admitted to the paediatric ward during the school summer holiday period to avoid missing time at school.
At admission her treatment regimen comprised Metformin 1000mg twice daily, Levemir insulin 16 units and Novorapid insulin 7 units with each meal. Her basal insulin had been changed just prior to admission to Levemir insulin from Degludec insulin to enable more responsive dose adjustments. She was commenced on a liquid diet from admission. Novorapid doses were calculated based on a 1:10g carbohydrate ratio (2 units per shake).
A libre 2 subcutaneous glucose sensor was used by our patient to help monitor glucose levels as well as intermittent finger prick blood glucose measurements.
During her admission our patient was reviewed by a diabetes specialist dietitian regularly, to monitor progress and support motivation. The diabetes consultant, specialist nurse and ward nursing staff also provided intensive support.
A daily exercise programme was devised by the paediatric physiotherapy team for our patient which she adhered to throughout the admission.
The ward play team provided activities and emotional support.
Progress during the admission and following discharge home
On day 4 of the admission our patient reported that she was struggling with the meal replacement shakes and was not managing the prescribed volume. Encouragement by the ward nursing staff and diabetes team was essential to support her to continue with the dietary plan. Insulin doses had been reduced to Levemir 10 units and Novorapid 2 units with each shake by this stage and blood glucose levels were stable at 4-8mmol/L with no hypoglycaemic episodes.
By day 10 of the admission insulin had been stopped completely and our patient was only taking Metformin 1000mg BD to maintain blood sugars in a 4-8mmol/l range. She had achieved a weight loss of 2kg.
The GLP1 agonist, Semaglutide was started on day 10 of admission. Semaglutide is currently licenced for young people aged 18 years and over but is used in younger children for obesity management by the local tertiary obesity service in Southampton. The use of Semaglutide in our patient was recommended by the tertiary obesity specialist team due to its effectiveness in weight reduction and appetite suppression and for the advantage that it only needs to be administered on a once weekly basis.
Appetite suppression on the lower dose of Semaglutide 0.5mg weekly was achieved for our patient. Our patient continued to struggle to tolerate the meal replacement shakes and on day 15 of admission it was agreed that she could reduce the volume of the milk added to the powder and her lunch time shake was replaced with a normal meal (300kcal).
On day 16 our patient was discharged home to continue the treatment plan. She had lost 2.2kg in weight during this admission.
A home visit by the dietitian to review progress was carried out at 12 days following discharge from hospital. Our patient had remained fully compliant with the dietary plan and was delighted that the intervention had been successful.
Her dose of Metformin was reduced by half and stopped by 4 weeks following discharge.
She continues on weekly Semaglutide 0.5mg and has not required insulin (4 months post discharge from hospital). Blood sugars have remained in a normal range.
At 11 weeks following the intervention our patient’s weight and BMI have reduced: weight 72.6kg to 61.9kg, BMI 30.9 kg/ m2 to 26.3kg/m2 (Figure 1 and 2) and her HbA1c has also reduced from 70mmol/mol to 43mmol/mol (non-diabetic range) (Figure 3).
We have also facilitated a reduced gym membership fee to a local gym for our patient and have encouraged her to take advantage of this.
SUMMARY
We have demonstrated that the intervention of a reduced calorie liquid diet can reverse type 2 diabetes and eliminate the need for insulin. Maintaining a low-calorie diet in the longer term can be very difficult but this has been achieved successfully in our patient with the use of the GLP1 agonist Semaglutide.
The success for our patient has been achieved in a secondary care setting by a 2-week hospital admission and an intensive multidisciplinary team effort. Our patient and her family were committed to and fully engaged with the treatment plan at the outset. Our patient has reported that although the initial hospital admission was very hard for her at times, she is very happy with the intervention and that her life is much better now that she doesn’t have to have 4 insulin injections per day. She will require long term regular follow up and we are hopeful that she will continue to maintain normal glycaemic control and thus significantly reduce her risks of long-term complications associated with type 2 diabetes.
We hope that this case report will encourage others to consider treatment of type 2 diabetes in children and young people with a low calorie diet intervention and become familiar and confident with the use of the newer anti-obesity drugs available.
Appendix 1 – dietary plan Patient/carer information leaflet A Low Calorie Diet
Leading studies has shown that for some people, type 2 diabetes can be put into remission by a substantial weight loss.
How much you need to lose depends on your starting body mass index (BMI). The weight loss diet is a 5 week low calorie diet (LCD, 1200kcal per day). It is important to bear in mind that the diet is only a few weeks long, it is followed by a return to normal eating but with reduced calorie intake than previously. You will not be missing out on things for too long! For this diet to be successful, it is important to stick to 1200kcal a day for a period of 4 weeks. It isn’t easy and is not right for everyone.
The liquid diet involves 2 phases:
Phase 1 - NO SOLID FOOD is eaten for 2 weeks, liquid replacement only.
Phase 2 - food is gradually reintroduced over a further 4 weeks to achieve a 1200-1400kcal diet of solid foods. After this phase you can discuss increasing your calorie intake with your dietitian back to estimated requirements of 2000kcal per day.
To follow this diet effectively you need to be committed for 6 weeks.
Your dietitian is: xxxxxxxx
If you have any queries or concerns contact them on: xxxxxxxxxxxxxxxxxx
A Low Calorie Diet
PHASE 1 Liquids only – NO FOOD
|
Advantages |
Disadvantages |
|
Doesn’t involve any food planning or cooking, which therefore removes some of the temptations. They are also easy to have ‘on the go’. |
Initially you may experience symptoms like headache, dizziness, tiredness and hunger but these are expected to wear off after a few days once your body adjusts. |
|
A complete break from old eating habits and behaviours so at the end of 8 weeks you can begin creating new eating habits when you begin to reintroduce foods. |
Increased risk of constipation, although this can be managed and prevented by ensuring an adequate fluid intake and taking a fibre supplement if required. |
|
The shakes are quick and easy to prepare, come in a variety of flavours, and are nutritionally complete when taken with a multivitamin. |
Some people may experience hair loss/thinning but this is usually only temporary, and hair will re-grow. |
|
Weight loss is expected due to the calorie deficit created and it can be very motivating to see results quickly, especially if it allows you to come off some of your medications too. |
You may experience an increased sensitivity to the cold, so are advised to wrap up warmly and include warm fluids. The soup sachets in the colder months can be useful. |
|
It can be cost effective as it works out cheaper than doing a weekly food shop, especially if using a supermarket own brand (see our suggestions below). |
It can be socially isolating. You may need a lot of support from your friends and family. |
How to do it
Use a meal replacement product: shakes, 4 individual sachets, each providing approximately 250-300 calories. This provides a total of 1000-1200kcal per day when prepared correctly, plus 1 additional serving of whole milk if required. You must have all the shakes to ensure you are getting all the essential vitamins and minerals required to prevent nutritional deficiencies. Have these instead of your usual meals/snacks. The only equipment you need is a shake mixer cup.
|
Weeks 1 and 2 |
|
|
Week 1 start date: ______ Week 2 start date: _____ |
During phase 1 you should have the following every day:
|
Example daily plan, depending on which shake is chosen.
|
8am: |
Meal replacement (250ml) |
|
9am: |
Sugar free drink (200ml) |
|
11am: |
Sugar free drink (200ml) |
|
12 noon: |
Meal replacement (250ml) |
|
1pm: |
Sugar free drink (200ml) |
|
3pm: |
Whole milk (200ml) |
|
5pm: |
Meal replacement (250ml) |
|
6pm: |
Sugar free drink (200ml) |
|
8pm: |
Meal replacement (250ml) |
|
9pm: |
Sugar free drink (200ml) |
The volume of the shake will depend on which one is chosen; see the table at the end of this document.
Steps to take before starting the diet
- As far as possible, remove all tempting foods from the house
- Discuss the diet with your family and close friends
- It would also be helpful not to eat meals away from home all the time. You may wish to have your drink with your family so you can still share in meal times.
- Think about how you might manage any social occasions. If you are invited out for a meal, you should explain the diet to them so they are aware you will not be eating any solid foods
- When reintroducing foods you should plan your meals in advance
- Write a shopping list and buy everything you will need before you start
e.g.
- your meal replacements
- milk to make up meal replacement if required (see instructions on pack)
- your sugar free fluid e.g. diet soft drinks, herbal teas,sugar-free squash
Frequently Asked Questions
Which meal replacements can I use?
|
Choose a product that matches the criteria below (all values are calculated after the shake or soup has been made with either milk or water as per the manufacturer’s guidance):
|
Suggested examples: **
with skimmed milk
with skimmed milk
up with water
make up with water
up with water |
**If you have any dietary intolerances/preferences please check with a dietitian as there are some products which may not be suitable and they can recommend alternatives.
Please note that none of these products are funded by the NHS in Hampshire.
Prices will vary depending on special offers and it is best to shop around. Buying a tub of powder and making them up yourself often works out cheaper.
Do I need additional supplements?
Yes, you will need to take an additional vitamin supplement. If iron deficiency anaemia is suspected prior to starting then your iron status should be assessed by your GP.
What sugar-free drinks can I have?
You must drink sugar free fluids in addition to your meal
replacements. You can have:
- plain water
- carbonated water
- soda water (check the label to ensure it has no added sugar)
- flavoured water (check the label to ensure it has no added sugar)
- herbal teas (e.g. mint, lemon & ginger)
- diet or zero fizzy drinks
- no added sugar squash
- sugar free squash
- tea/coffee (you can use milk from your daily allowance of 100ml & add sweetener but not sugar)
Why not add a slice of lemon or lime to your water to make it more refreshing?
Will I have any side effects?
A small number of patients may experience mild side effects whilst on this diet. The most common side effect is constipation.
Please contact your Dietitian if you suffer any extreme side effects from this diet.
What should I do if I get constipated?
If after 1-2 days you find this is becoming a problem then we recommend that you take Optifibre to relieve these symptoms.
Do I need to monitor my blood glucose levels?
Yes, you will need to check on waking, before each shake, 2 hours after each shake and before bed.
Please contact your diabetes health care professional if:
- Your blood glucose levels are above 14mmol/l on waking or before meals
- Your blood glucose levels are below 4mmol/l (hypo) or you are having any hypo symptoms.
Do any of my medications need adjusting?
Your health care professionals will interpret and help you manage your diabetes and any related complications in light of your individual circumstances and adjust your medication accordingly.
Other diabetes medication:
All other oral medications can be decreased or stopped in agreement with your health care professional dependent on how well your diabetes control improves.
Meal replacement shakes are not a long-term solution for weight management. Long-term weight loss requires a significant change in lifestyle, including altering the composition of the diet. This is when phase 2 begins, the re-introduction of food and healthy eating behaviours with which you can also be supported.
Leslie WS, Ford I, Sattar N, Hollingsworth KG, Adamson A, Sniehotta FF, McCombie L, Brosnahan N, Ross H, Mathers JC, Peters C, Thom G, Barnes A, Kean S, McIlvenna Y, Rodrigues A, Rehackova L, Zhyzhneuskaya S, Taylor R, Lean ME. The Diabetes Remission Clinical Trial (DiRECT): protocol for a cluster randomised trial. BMC Fam Pract. 2016 Feb 16;17:20.
PHASE 2 (weeks 3-6) Food Reintroduction
During phase 2 you will start to introduce food whilst reducing your milk intake. As a general guide when re-introducing meals have ¾ of what you used to eat. In summary each week you will re-introduce a meal or snacks.
|
Week 3 INTRODUCE LUNCH Start date: |
Have the following every day:
|
|
Week 4 INTRODUCE EVENING MEAL Start date: |
Have the following every day:
|
|
Week 5 INTRODUCE BREAKFAST + 1 x SNACK Start date: |
Have the following every day:
|
|
Week 6 INTRODUCE 1 MORE SNACK |
Have the following every day:
2 litres of other sugar free fluid |
EVENING MEAL (400 kcal)
This meal must include:
- 100g (4oz) lean meat or 125g (5oz) plain white fish/ tinned tuna or 150g (6oz) plain prawns or 2 boiled eggs or 150g (6oz) Quorn mince
- 4 egg size potatoes (185g/7.5oz cooked) or 4 tbsp cooked plain rice/cous cous (50g/2oz/2tbsp uncooked) or 6 tbsp cooked plain pasta (50g/2oz uncooked)
- ½ plate of salad or vegetables
- One piece of fruit
Optional - gravy (instant – with no added meat juices!) or one dessertspoon of low fat salad dressing/ketchup/ pickle
Tips
- Do not add fats when cooking - prepare foods by dry- frying, dry-roasting, stewing, grilling, boiling, steaming
- Add extra flavour without adding calories e.g. use garlic, chilli, lemon juice, pepper, curry powder, herbs, spices
- Add flavour to salads with lemon juice or balsamic vinegar
- Have the fruit as a dessert – why not chop and add to one of your yoghurts?
Meal ideas
|
Roast
|
|
Fish
|
|
Chilli
|
|
Fish pasta
|
|
Curry
|
|
Spicy chicken
|
BREAKFAST (300Kcal)
Choose one of the following for breakfast:
|
Breakfast cereal 6tbsp cereal (40g) (e.g. branflakes, cornflakes, All Bran) or 2 weetabix/shredded wheat or 4tbsp plain oats/muesli (no added sugar varieties) Serve with 1/3 pint (200ml) semi-skimmed milk |
|
or |
|
Toast 2 slices of toast (medium cut) topped with one of the following:
|
|
or |
|
Crackers 4 oatcakes or 5 Ryvita (original) or 5 plain rice cakesTop with low fat cheese spread (60g), or a scraping of low fat spread, marmite or jam |
LUNCH (300Kcal)
Choose one of the following for lunch:
|
Sandwich 2 slices of bread (medium cut) or 1 pitta or 1 small roll filled one of the following:
2 grilled slices of lean bacon |
|
Toast toppers 2 slices of toast (medium cut) topped with one of the following:
100g (4oz) tinned sardines, mackerel or pilchards (in tomato or mustard sauce) |
|
Omelette 2 egg omelette cooked with onions, mushrooms, peppers and tomatoes. Serve with 2 slices bread (medium cut) or 4 egg sized boiled potatoes |
|
Crackers 4 oatcakes or 5 Ryvita/plain rice cakes with one of the following:
|
|
Jacket potato One potato (the size of your fist) with one of the following toppings:
|
Tips
- Add plenty of salad or veg to your lunch e.g. salad leaves, radish, cucumber, celery, beetroot, mushrooms, pepper, grated carrot, spring onion, pickled onions, fresh or tinned tomatoes – aim for ½ plate
- Watch your added fats – do not add fats when cooking and do not add more than 2 tsp low fat spread or 2 tsp low fat mayo/salad cream or 1 dessert spoon of low fat salad dressing/ketchup/pickle/brown sauce
- Dress salads with lemon juice or balsamic vinegar for no extra calories
SNACKS - Choose ONE of the following snacks each day (Total 200kcal):
|
Sweet 1 sugar free jelly 2 pieces of fruit 1 tablespoon of raisins/sultanas 6 dried apricots 1 small slice of malt loaf (no butter!) or finger of cake 1 Muller lite or Shape/Activia 0% 2 Rich Tea, Ginger Nuts biscuits or Jaffa Cakes 1 hob nob or chocolate digestive 2 finger KitKat 1 bite-size Brownie or mini chocolate roll 1 small meringue nest with a handful of berries 2 low calorie hot chocolate drinks ½ mini apple pie or bakewell tart 1 crumpet with a scraping of jam (no butter!) 1 weetabix or 1 shredded wheat with semi-skimmed milk 3 tablespoons of cereal with semi- skimmed milk |
Savoury 1 slice of toast (medium cut - no spread) with 2 tinned tomatoes 1 slice of bread (medium cut - no spread) with marmite or scraping of low fat cheese spread 2 original Ryvita/plain rice cakes topped with scraping of marmite or low fat cheese spread & tomatoes/ cucumber or 100g tomato salsa 1 original Ryvita/rice cake with 100g fat free cottage cheese/50g low fat cottage cheese & 7 cherry tomatoes 1 original Ryvita/rice cake topped with a sliced boiled egg 1 mini pitta/½ standard pitta filled with lots of salad or scraping of low fat cheese spread or marmite 2 oat cakes & 7 cherry tomatoes 1 small packet of Quavers, Skips, Twiglets or reduced fat crisps |
Tip: Plan your snacks when you most likely feel the need to eat e.g. evening time, mid-afternoon
Meal Replacements
|
|
Kcal/ shake |
Shakes |
No per day |
Fluid |
|
Approx cost per day |
|
Slim fast Powder |
300 |
Y |
4 |
250 |
Add 250ml whole milk |
£3.00 |
|
Slimfast (ready to drink) |
204 |
Y |
5 + 300ml milk |
325 |
Pre made |
£9.50 |
|
Ultra slim (Tesco) |
250 |
Y |
4 + 200ml milk |
200 |
Add 215ml whole milk |
£2.00 |
|
Shake that weight |
292 |
Y |
4 |
250 |
250ml whole milk |
£6-7 |
|
Asda Great Shape Shakes |
250 |
Y |
4 + 200ml milk |
250 |
Add 215ml whole milk |
£2.00 |