Recent Articles
-
February 02, 2024 Research Article
 Abstract Background: Chronic Kidney Diseases (CKD) is a progressive, irreversible loss of kidney function with great debilitations to the patient and the cost of health care for individuals, their families and a countries overall healthcare cost. The preventi.....
Abstract Background: Chronic Kidney Diseases (CKD) is a progressive, irreversible loss of kidney function with great debilitations to the patient and the cost of health care for individuals, their families and a countries overall healthcare cost. The preventi..... -
February 23, 2024 Review Article
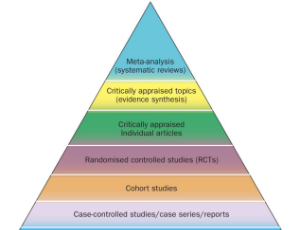 Abstract Within the pyramid of evidence, systematic reviews are at the top. Systematic review articles must be carefully crafted if they are to convey the broad range of research activities effectively and briefly. This necessitates close consideration of m.....
Abstract Within the pyramid of evidence, systematic reviews are at the top. Systematic review articles must be carefully crafted if they are to convey the broad range of research activities effectively and briefly. This necessitates close consideration of m..... -
January 22, 2024 Case Report
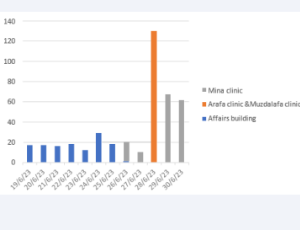 Abstract Mass gathering events pose significant healthcare challenges, including the spread of infectious diseases, strain on local medical resources, and the high density of participants.
Abstract Mass gathering events pose significant healthcare challenges, including the spread of infectious diseases, strain on local medical resources, and the high density of participants. -
December 25, 2023 Research Article
 Abstract Aim: To determine the subjective quality of life and associated factors among visually impaired patients in Ogbomoso. Objectives: A: To determine the subjective quality of life among visually impaired patients in Ogbomoso (considering sustainable dev.....
Abstract Aim: To determine the subjective quality of life and associated factors among visually impaired patients in Ogbomoso. Objectives: A: To determine the subjective quality of life among visually impaired patients in Ogbomoso (considering sustainable dev..... -
November 29, 2023 Review Article
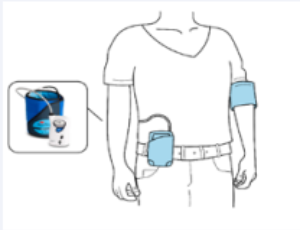
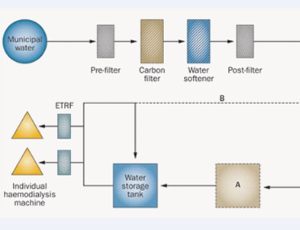 Abstract Arid and semi-arid regions are increasingly facing a major water shortage problem. As the population increases in these regions, water is becoming more and more precious with very limited resources in Near East and North Africa region (NENA). Hemodia.....
Abstract Arid and semi-arid regions are increasingly facing a major water shortage problem. As the population increases in these regions, water is becoming more and more precious with very limited resources in Near East and North Africa region (NENA). Hemodia..... -
November 29, 2023 Commentary
 Abstract The Food and Drug Administration (FDA) mandated that beginning September 10, 2024, every screening mammogram report include an assessment of Breast Density (BD), which must be communicated to the patient [1]. As the ordering clinician, Family Medicin.....
Abstract The Food and Drug Administration (FDA) mandated that beginning September 10, 2024, every screening mammogram report include an assessment of Breast Density (BD), which must be communicated to the patient [1]. As the ordering clinician, Family Medicin..... -
November 10, 2023 Research Article
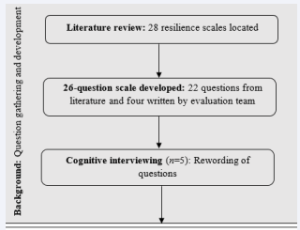 Abstract Background: The Adolescent Family Life Program Positive Youth Development (AFLP PYD) model is a case management-based intervention that supports the development of protective factors that contribute to resilience among Expectant and Parenting Youth (.....
Abstract Background: The Adolescent Family Life Program Positive Youth Development (AFLP PYD) model is a case management-based intervention that supports the development of protective factors that contribute to resilience among Expectant and Parenting Youth (..... -
August 03, 2023 Research Article
 Abstract Purpose: The purpose of this study was to evaluate the feasibility and preliminary effectiveness of implementing a self-administered acupressure intervention for chronic low back pain (CLBP) relief among patients in a community free clinic in the Met.....
Abstract Purpose: The purpose of this study was to evaluate the feasibility and preliminary effectiveness of implementing a self-administered acupressure intervention for chronic low back pain (CLBP) relief among patients in a community free clinic in the Met..... -
October 09, 2023 Research Article
 Abstract Background: Intimate Partner Violence (IPV) is a preventable public health problem and one of the most common types of violence against pregnant women which could be a cause of perinatal and maternal morbidities and mortalities. Screening for IPV dur.....
Abstract Background: Intimate Partner Violence (IPV) is a preventable public health problem and one of the most common types of violence against pregnant women which could be a cause of perinatal and maternal morbidities and mortalities. Screening for IPV dur..... -
September 23, 2023 Case Report
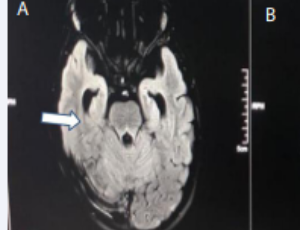 Abstract Lower Motor Nerve (LMN) facial palsy is a rare presentation of systemic hypertension in children. A 8.5 year old boy, initially had isolated right LMN facial palsy, progressed over 2 weeks to hypertensive encephalopathy, obstructive hydrocephalous, s.....
Abstract Lower Motor Nerve (LMN) facial palsy is a rare presentation of systemic hypertension in children. A 8.5 year old boy, initially had isolated right LMN facial palsy, progressed over 2 weeks to hypertensive encephalopathy, obstructive hydrocephalous, s..... -
August 03, 2023 Research Article
 Abstract Abstract Background: Maternal deaths remain excessively high in developing countries, particularly in sub-Saharan Africa. In Nigeria, the Maternal Mortality Rate (MMR) ranged from 448 to 4210 per 100,000 live births with hypertensive disorders and ha.....
Abstract Abstract Background: Maternal deaths remain excessively high in developing countries, particularly in sub-Saharan Africa. In Nigeria, the Maternal Mortality Rate (MMR) ranged from 448 to 4210 per 100,000 live births with hypertensive disorders and ha..... -
December 11, 2015 Short Communication
 Abstract With the advancement in technology, many couples with infertility choose in vitro Fertilization (IVF) treatment as a significant mean to achieve their dream of parenthood. However, with very low success rate, many of them face treatment failures and .....
Abstract With the advancement in technology, many couples with infertility choose in vitro Fertilization (IVF) treatment as a significant mean to achieve their dream of parenthood. However, with very low success rate, many of them face treatment failures and .....