Success with Modified ERCP In Patients with Gastric Bypass
- 1. Fellow resident. Bariatric Surgery. Instituto Nacional de Ciencias Médicas y Nutrición. Mexico City
- 2. Bariatric and Endocrine Surgeon. Instituto Nacional de Ciencias Médicas y Nutrición. Mexico City
- 3. American British Cowdray Medical Center IAP, Center for Nutrition and Obesity. Mexico City
ABSTRACT
Introduction: Obesity is a complex multifactorial phenotype; inter-individual variation in such phenotypes is thought to result from the action of multiple genes and environmental factors. Bariatric surgery provides the most efficient and sustained treatment for morbid obesity. Roux en-Y-gastris bypass (RYGPB) is a lithogenic risk factor due to rapid weight loss. The lithogenic effect of rapid weight loss is seen as early as four weeks although it generally appears within 7-18 months. Other complications of cholelithiasis (i.e., acute cholecystitis, choledocholithiasis, cholestatic jaundice, acute cholangitis, acute pancreatitis) might increase as well during obesity or rapid weight loss, as gallstone prevalence also increases. The presence of gallstones in the common bile duct (CBD) although is a rare complication after RYGBP, represents an important challenge due to the anatomical modifications of the gastrointestinal tract. A solution that has been found to access the excluded stomach through laparoscopy and inserting the endoscope through a gastrotomy allowing to perform an ERCP like in a traditional way.
Objective: We present two cases of patients with a history of gastric bypass who presented bile duct obstruction and we performed laparoscopic-assisted ERCP.
Results: We present 2 patients with history of RYGB who underwent laparoscopic assisted transgastric ERCP. The mean body mass index after RYGB was 31 kg/m2 . ERCP was performed to manage choledocholitiasis within 6-7 years (mean 78 months) of RYGB surgery. The mean duration of the procedure was 185 ± 25 min; the average hospital stay was 2.5 ± .5 days. No complications were develop after the procedure.
Conclusions: transgastric endoscopic retrograde cholangiopancreatography is safe and feasible for the management of biliary tract disease in patients with history of Rouxen-Y gastric bypass.
KEYWORDS
Gastric bypass; Choledocholithiasis;ERCP; Laparoscopy.
CITATION
Pimienta-Sosa AP, Herrera-Hernández MF, Pantoja-Millan JP, Sierra-Salazar M (2021) Success with Modified ERCP In Patients with Gastric Bypass. JSM Surg Proced 2(1): 1003.
INTRODUCTION
Obesity is a complex multifactorial phenotype; interindividual variation in such phenotypes is thought to result from the action of multiple genes and environmental factors (1). In Mexico, overweight and obesity represent a serious public health problem, affecting 7 out of every 10 adults from different regions, localities and socioeconomic status (2). The prevalence of overweight and obesity in Mexican children and adults has increased alarmingly in the last two decades, today, 70% of Mexicans are overweight and almost a third suffer from obesity (3). One of the many complications of obesity is cholelithiasis. In women, there is a strong positive correlation between body mass index (in kg/m2 of surface area) and the relative risk of gallstones. In one study, the age-adjusted relative risk in slightly overweight women (24-25 kg/m2 ) was 1.7 compared to normal weight persons and this is increased to 6.0 in women who were markedly overweight (32 kg/m2 ) (4). The association of gallstones with obesity in men has been more difficult to show. Some studies indicated that body mass index (BMI) was no different in men with or wihout gallstones, irrespective of age (5,6). Most gallstones in obese persons are cholesterol stones. Three major factors have been implicated in the formation of cholesterol stones: the supersaturation of bile with cholesterol, a nucleation defect and impaired gallbladder motility (7). Regional distribution of fat may also be of importance. Also, gallstones in obese persons seem to be frequently symptomatic (8). Bariatric surgery provides the most efficient and sustained treatment for morbid obesity. It is well known that weight loss surgery decreases both morbidity and mortality in obese patients. However, the formation of gallstones in these patients remains a subject of concern (9,10). There continues to be a controversy over whether routine prophylactic cholecystectomy should be performed during Roux-en-Y gastric bypass (RYGBP) surgery. Several alternative approaches have been suggested regarding the management of the gallbladder during bariatric surgery; these include cholecystectomy only after preoperatively detected gallbladder pathology by ultrasound, cholecystectomy after intraoperative verification of gallstones with ultrasound, routine administration of ursodeoxycholic acid to all patients to prevent gallstone formation, and no treatment for asymptomatic patients before or after surgery (11). A selective approach using intra-operative ultrasoundand selective cholecystectomy followed by prophylactic ursodeoxycholic acid has been advocated by Scott et al. (12). but compliance with the ursodiol was only 41%. It does appear that combined laparoscopic RYGBP with cholecystectomy is safe and feasible without altering port placement; however, it does increase operative time and hospital length of stay (13). Cholecystectomy following RYGBP surgery may present some technical challenges to the surgeon. Adhesions that occur following foregut surgery could make laparoscopic visualization of the anatomy more difficult. In addition, with RYGBP it is much less feasible or impossible to perform endoscopic pancreatic cholangiopancreatography (ERCP) if needed, following the creation of the long Roux limb(14). RYGPB is a lithogenic risk factor due to rapid weight loss. The lithogenic effect of rapid weight loss is seen as early as four weeks although it generally appears within 7-18 months. The risk of becoming symptomatic ranges from 28% to 71% after gastric bypass procedure and this requires urgent cholecystectomy in up to one-third of patients by three years(15). Other complications of cholelithiasis (i.e., acute cholecystitis, choledocholithiasis, cholestatic jaundice, acute cholangitis, acute pancreatitis) might increase as well during obesity or rapid weight loss, as gallstone prevalence also increases (16). The presence of gallstones in the common bile duct (CBD) although is a rare complication after RYGBP (around 0.2% of the bariatric patients) represents an important challenge due to the anatomical modifications of the gastrointestinal tract. The duodenum remains adjacent to the surgically excluded stomach. Therefore, for the endoscopist, accessing the ampulla is technically very difficult. The endoscope must pass through the mouth, esophagus, gastric pouch, Roux limb, and then return retrograde through the afferent limb to reach the ampulla. This total length may easily exceed 300 cm, making almost impossible for traditional endoscopy access to the papilla to perform an ERCP(17). Due to the long anatomical route required to reach the biliopancreatic limb in patients with RYGBP, a solution that has been found to access the excluded stomach through laparoscopy and inserting the endoscope through a gastrotomy allowing to perform an ERCP like in a traditional way.
PATIENTS AND METHODS
This is a retrospective study; using our database, we present two patients who developed common bile duct obstruction after gastric bypass and underwent laparoscopic-assisted. ERCP. Patient Characteristics Both patients were female. The average age was 46.5. The mean body mass index (BMI) of the patients after bariatricsurgery was 31 kg/m2 ; the average time elapsed between the RYGB and ERCP procedure was 78 months (Table 1).
Table 1: Patient characteristics, including demographics, BMI, and time elapsed between RYGB and ERCP.
| Patient no. | Age (years) | Gender | CVL transop. | BMI (kg/m² | Time between RYGB and ERCP (months) |
| 1 | 52 | F | No | 29 | 72 |
| 2 | 41 | F | No | 33 | 84 |
F female, RYGB gastric bypass Roux-en-Y, CVL laparoscopic cholecystectomy, BMI body mass index, ERCP endoscopic retrograde cholangiopancreatography
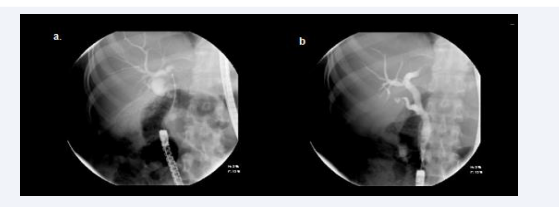
Surgical Technique In this procedure a standard laparoscopic access to the abdominal cavity is performed with a Veress needle an then making four incisions. We inserted a 12-mm umbilical trocar for vision,on the anterior axillary line and in the left subcostal region for the duodenoscope. A 5-mm trocar was inserted in the right sub- costa region. After identifying and dissecting any adherences on the anterior wall, the greater curve of the antrum in the gastric remnant is mobilized and a gastrotomy and purse-string suture are fashioned on the anterior side of the greater curvature of the gastric remnant. This purse-string has to be tightly fixed around a 12mm trocar to prevent loss of insufflation pressure, and the gastrotomy should be made as lateral as possible along the greater curvature to permit smooth intubation of the pylorus. It’s also recommended to occlude the biliopancreatic limb with an intestinal clamp to prevent over-insufflation of the small bowel that blocks the perioperative visualization.Finally, a side-viewing duodenoscope is introduced through the 12 mm trocar secured into the gastrotomy, and ERCP can be performed under fluoroscopic guidance (Figure 1).
Figure 1 Endoscopic retrograde cholangiography performed through the gastrostomy track created.
The endoscope was passed through the gastrotomy and progressed through the pylorus as far as the dupdenal papilla. The traditional method used for papillotomy was performed for cannulation and treatment of the biliary and pancreatic ducts. After conclusion of the ERCP and removal of the scope, the gastrotomy was closed in two planes with 3-0 absorbable sutures. The trocars were removed under laparoscopic vision, and the incisions in the skin were sutured with non-absorbable sutures.
Statistical Analysis The statistical analysis was performed with the SPSS program. The results of quantitative variables were presented as the mean ± SD.
RESULTS
In this retrospective study we evaluated 2 patients what were treated with a laparoscopic-assisted ERCP. The procedure resulted in a 100% success rate (Table 2).
Table 2: Results of the ERCP procedure.
| Patient no | Clinical indication | US findings | ERCP findings | Intervention | Surgical time(min) | Hospitalization (days) |
| 1 | Obst. jaundice | CDL | CDL | SP + BSR | 160 | 3 |
| 2 | Obst. jaundice | Dilation BT + CDL | CDL | SP + BSR | 210 | 2 |
CDL choledocholithiasis, SP sphincterotomy, BT biliary tract, Obst. jaundice obstructive jaundice, BSR bile duct stone removal
The most common clinical pathology found was choledocholitiasis. The diagnosis was confirmed by magnetic resonance cholangiopancreatography and ultrasound scans. In both cases, the ERCP procedure was concluded without intraoperative complications. No pancreatitis was seen after ERCP procedure. The mean duration of the procedure was 185 ± 25 min. and the mean period of hospitalization was 2.5 ± .5 days. Both patients exhibited normal clinical and laboratory results 3 and 6 months after the procedure.
DISCUSSION
Laparoscopic approached for ERCP are becoming more frequently reported in patients with history of gastric bypass. The interaction between the surgeon and the endoscopist is fundamental for the success of this procedure (18).
Two major limitations to the oral approach for the ERCP after RYGB are the sparse availability of adequate accessories for the execution of procedures on the papilla and the inverted position of the mayor ampulla (19).
In our experience, the transgastric laparoscopic approach with a duodenoscope was 100% successful in locating and examining the papilla. This was comparable to the results chieved by Nguyen et al(20).
Matlock et al. used a laparoscopic approach with a gastrotomy in 10 patients after RYGB and achieved 100% success in the catheterization of the biliary tract(21)
Choledocholitiasis was the principal and most common clinical diagnosis in the present series. Access to the biliopancreatic tract with laparoscopic assistance has been shown to be both safe and highly successful in patients after RYGB.
Despute the inherent risk involved in anesthesia and laparoscopic surgery, no mortality has been reported. The disadvantages of this approach rate are the need for a larger surgical/endoscopic team, the relatively long period required for execution, and consequently the higher cost(22).
CONCLUSION
These cases demonstrated that transgastric endoscopic retrograde cholangiopancreatography is safe and feasible for the management of biliary tract disease in patients with history of Roux-en-Y gastric bypass.