Recent Articles
-
December 03, 2025 Review Article
 Abstract CT-derived fractional flow reserve (FFR-CT) is a noninvasive technique that combines coronary computed tomography angiography (CCTA), with computational modeling to assess the physiological significance of coronary artery stenoses. By integrating a.....
Abstract CT-derived fractional flow reserve (FFR-CT) is a noninvasive technique that combines coronary computed tomography angiography (CCTA), with computational modeling to assess the physiological significance of coronary artery stenoses. By integrating a..... -
November 21, 2025 Review Article
 Abstract Acute chest pain is one of the most common reasons for emergency department (ED) visits, yet only a small fraction of cases are due to acute coronary syndrome (ACS), creating a diagnostic challenge. Traditional evaluation methods including clinical a.....
Abstract Acute chest pain is one of the most common reasons for emergency department (ED) visits, yet only a small fraction of cases are due to acute coronary syndrome (ACS), creating a diagnostic challenge. Traditional evaluation methods including clinical a..... -
October 02, 2025 Research Article
 Abstract Objective: To investigate the value of a mechanical learning model based on multiparametric MRI imaging histology combined with clinical and conventional radiological features for preoperative prediction of perineural invasion (PNI) in rectal cance.....
Abstract Objective: To investigate the value of a mechanical learning model based on multiparametric MRI imaging histology combined with clinical and conventional radiological features for preoperative prediction of perineural invasion (PNI) in rectal cance..... -
September 14, 2025 Research Article
 Abstract Background: Developmental delays in children may result from a variety of neurological adverse effects on the developing brain. One of the most important methods for assessing children with developmental delay is neuroimaging, specifically magneti.....
Abstract Background: Developmental delays in children may result from a variety of neurological adverse effects on the developing brain. One of the most important methods for assessing children with developmental delay is neuroimaging, specifically magneti..... -
September 04, 2025 Research Article
 Abstract Objectives: To correlate the texture analysis (TA) parameters of temporomandibular joint (TMJ) articular disc images with the clinical and imaging characteristics of patients with temporomandibular disorder (TMD). Methods: A total of 110 Magneti.....
Abstract Objectives: To correlate the texture analysis (TA) parameters of temporomandibular joint (TMJ) articular disc images with the clinical and imaging characteristics of patients with temporomandibular disorder (TMD). Methods: A total of 110 Magneti..... -
August 01, 2025 Research Article
-
June 21, 2025 Research Article
 Abstract Objectives: An early and precise diagnosis is important to confirm acute appendicitis (AA) in children. Ultrasound imaging techniques have demonstrated higher value in the diagnosis of AA. This study was conducted to ascertain the nondiagnostic and.....
Abstract Objectives: An early and precise diagnosis is important to confirm acute appendicitis (AA) in children. Ultrasound imaging techniques have demonstrated higher value in the diagnosis of AA. This study was conducted to ascertain the nondiagnostic and..... -
July 03, 2025 Review Article
 Abstract Heterotopic Ossification (HO) is a distinct clinico-radiological entity acccounting for post treatment morbidity in post arthroplasty and trauma patients. Radiotherapy is an effective modality for prophylactic treatment in this condition. The corr.....
Abstract Heterotopic Ossification (HO) is a distinct clinico-radiological entity acccounting for post treatment morbidity in post arthroplasty and trauma patients. Radiotherapy is an effective modality for prophylactic treatment in this condition. The corr..... -
May 11, 2025 Case Report
 Abstract Schnitzler síndrome is a rare autoinflammatory disorder characterized by a combination of symptoms that include recurrent urticaria (hives), fever, joint pain, and the presence of a monoclonal IgM paraprotein in the blood.
Abstract Schnitzler síndrome is a rare autoinflammatory disorder characterized by a combination of symptoms that include recurrent urticaria (hives), fever, joint pain, and the presence of a monoclonal IgM paraprotein in the blood. -
May 07, 2025 Research Article
 Abstract To study the clinical features of the complicated forms of spinal hernias in combination with other malformations of the central nervous system Research. The research work was carried out in the clinic of the Children’s National Medical Center. The.....
Abstract To study the clinical features of the complicated forms of spinal hernias in combination with other malformations of the central nervous system Research. The research work was carried out in the clinic of the Children’s National Medical Center. The..... -
November 30, 2024 Review Article
 Abstract Radiation exposure is increasingly relevant in medical, environmental, and occupational contexts, bringing both benefits and health risks. This review evaluates the health impacts of ionizing and non-ionizing radiation, highlighting short- and lo.....
Abstract Radiation exposure is increasingly relevant in medical, environmental, and occupational contexts, bringing both benefits and health risks. This review evaluates the health impacts of ionizing and non-ionizing radiation, highlighting short- and lo..... -
October 25, 2024 Mini Review
 Abstract High-Resolution Computed Tomography (HRCT) has emerged as an invaluable tool for diagnosing and assessing pulmonary tuberculosis (TB) in patients. This research paper provides a comprehensive review of the role of HRCT in the evaluation of lung manif.....
Abstract High-Resolution Computed Tomography (HRCT) has emerged as an invaluable tool for diagnosing and assessing pulmonary tuberculosis (TB) in patients. This research paper provides a comprehensive review of the role of HRCT in the evaluation of lung manif..... -
October 03, 2024 Research Article
 Abstract Introduction: Intracranial cerebral arteriovenous malformations (AVMs) are congenital malformations. For patients with Grade ? or higher on the Spetzler- Martin grade, radiotherapy or vascular embolization combined with surgery is considered. Stereot.....
Abstract Introduction: Intracranial cerebral arteriovenous malformations (AVMs) are congenital malformations. For patients with Grade ? or higher on the Spetzler- Martin grade, radiotherapy or vascular embolization combined with surgery is considered. Stereot..... -
July 11, 2024 Review Article
 Abstract As we known, many compounds in the human body contain phosphorus which provides vital information on changes in cancer microenvironment. Phosphorous-31 (31P) magnetic resonance spectroscopy (MRS), as a powerful non-invasive tool, can be utilized in d.....
Abstract As we known, many compounds in the human body contain phosphorus which provides vital information on changes in cancer microenvironment. Phosphorous-31 (31P) magnetic resonance spectroscopy (MRS), as a powerful non-invasive tool, can be utilized in d..... -
March 22, 2024 Research Article
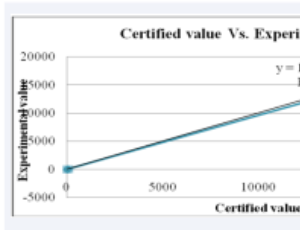 Abstract Kota Hare, Burii and Godere has exhibited many therapeutic activities. Trace elements are required by human body and any deviation from its optimal limits affects the general well-being of any individual. They may be responsible for therapeutic act.....
Abstract Kota Hare, Burii and Godere has exhibited many therapeutic activities. Trace elements are required by human body and any deviation from its optimal limits affects the general well-being of any individual. They may be responsible for therapeutic act..... -
August 24, 2013 Editorial
 Abstract Ferumoxytol (Feraheme ®) is an iron oxide nanoparticle approved by the Food and Drug administration (FDA) in 2009 for treating anemia, but has found excellent off-label uses as contrast agent in the magnetic resonance imaging (MRI) of many neurolog.....
Abstract Ferumoxytol (Feraheme ®) is an iron oxide nanoparticle approved by the Food and Drug administration (FDA) in 2009 for treating anemia, but has found excellent off-label uses as contrast agent in the magnetic resonance imaging (MRI) of many neurolog.....